Improving well being and reducing prices for the sickest and most costly sufferers in America is a dream more durable to comprehend than many well being care leaders had hoped, in line with a study published Wednesday by the New England Journal of Medicine.
Researchers examined whether or not pairing steadily hospitalized sufferers in Camden, New Jersey, with nurses and social employees may cease that pricey cycle of readmissions. The examine discovered no impact: Patients receiving additional assist had been simply as more likely to return to the hospital inside 180 days as these not receiving that assist.
The outcomes are a blow to Dr. Jeffrey Brenner and the Camden Coalition of Healthcare Providers, the group he based practically 20 years in the past.
“It’s my life’s work. So, of course, you’re upset and sad,” mentioned Brenner, who now does related work with medical health insurance big UnitedHealthcare.
The mannequin of care, pioneered partially by Brenner and profiled in a extensively learn 2011 article in The New Yorker, has impressed dozens of comparable initiatives throughout the nation and attracted thousands and thousands in philanthropic funding.
“This is the messy thing about science,” mentioned Brenner, who gained a MacArthur Foundation “Genius Grant” for his efforts. “Sometimes things work the way you want them to do work and sometimes they don’t.”
The Hope
Many hospital and insurance coverage executives have pinned their hopes on this work as a result of it promised to resolve a typical drawback: when sufferers lives are so difficult by social components like poverty and habit that their manageable medical situations, like diabetes and bronchial asthma, result in costly, recurring hospital stays.
Writer and doctor Atul Gawande launched Brenner as a brash visionary crusading on behalf of the “worst-of-the-worst patients” within the New Yorker piece, titled “The Hot Spotters.” (Gawande, who now heads Haven, a three way partnership of Amazon, Berkshire Hathaway and JPMorgan Chase, declined to be interviewed for this text.)
Brenner’s prescription: Pair these folks with front-line care employees who would shepherd them to the social and medical providers they wanted. Early proof was promising, the anecdotes inspiring. Brenner boiled the mannequin’s potential all the way down to 4 phrases and two tantalizing objectives: higher care, decrease prices.
As phrase unfold, breathless headlines popped up like “Health Care’s Best Hope” and “Could Camden Coalition Save US Healthcare?”
“Lots of organizations make claims that their programs work and they’ve never been rigorously tested,” Brenner mentioned.
Instead, Brenner took the bizarre step of inviting the scrutiny of revered researchers.
In 2014, Massachusetts Institute of Technology economist Amy Finkelstein started a randomized managed trial, the identical rigorous methodology used to judge new medication. Over 4 years, the coalition enrolled 800 sufferers, all who had been not too long ago hospitalized and struggled with social issues. Half obtained the same old care sufferers get when leaving the hospital. The different half received about 90 days of intensive social and medical help from the coalition.
And the outcome: The 400 sufferers who obtained the intensive assist had been simply as more likely to return to the hospital because the sufferers who didn’t. In each teams, practically two-thirds of individuals had been readmitted inside 180 days.
So why did the coalition fail? Why did the financial savings touted of their early information, which Gawande had declared “revolutionary” in The New Yorker practically a decade in the past, disappear when put to this rigorous take a look at?
Larry Moore is doing properly in the present day, however his story illustrates how tough it’s to deal with folks with advanced social and medical issues.
‘My Daily Routine’
Larry Moore, who has hypertension, alcohol habit, persistent seizures and issue strolling, was one of many first folks to enroll within the coalition’s trial.
Moore’s expertise serves as a street map for understanding why the coalition missed its mark.
His first months had been promising: prescriptions crammed, medical appointments attended, Social Security advantages declare in course of. The 47-year-old even began to belief the group with the small print of his deep-seated habit, confiding how he would eat mouthwash, vanilla extract and even hand sanitizer at instances.
“You couldn’t keep anything with alcohol in it” round him, Moore recalled. “That’s addiction.”
But all of the progress immediately stopped when Moore appeared to vanish from the coalition’s radar.
“We didn’t see Mr. Moore after November,” mentioned nurse Jeneen Skinner. “We went to the house. We sent text messages. We [made] phone calls.”
The coalition has realized that for folks dwelling in poverty and with poor well being, a small hiccup — in Moore’s case, a missed lease cost — can spiral into a significant setback.
Moore spent the subsequent 2½ years principally homeless, utterly out of contact with the coalition.
“I was going from place to place. I sleep on a bench or a rock until the next day when the liquor store opens,” remembered Moore. “That was my daily routine.”
Seventy emergency room visits and 6 hospital admissions later, Skinner reconnected with Moore.
He instructed her the one factor that may preserve him out of the hospital: housing.
The ‘Camden Coalition’
Too many instances, in the course of the trial, folks ended up again within the hospital regardless of the intervention. But the coalition is satisfied it didn’t fail as a lot because the bigger social security internet did.
“The bottom line is, we built a brilliant intervention to navigate people to nowhere,” mentioned Brenner.
Coalition workers and their sufferers often knew what was wanted — evidence-based habit remedy, housing, psychological well being providers — however assets had been typically briefly provide.
Over the previous three years, the coalition got down to fill in these gaps, present process a form of metamorphosis.
“We think of ourselves now as the Camden Coalition” steering away from the “health care providers” a part of the title, mentioned Kathleen Noonan, who succeeded Brenner as head of the group.
It has solid partnerships with jails, legal professionals and legislators, and began its personal housing program. Many of those efforts started because the scientific trial was ongoing — an indication the coalition had seen the writing on the wall.
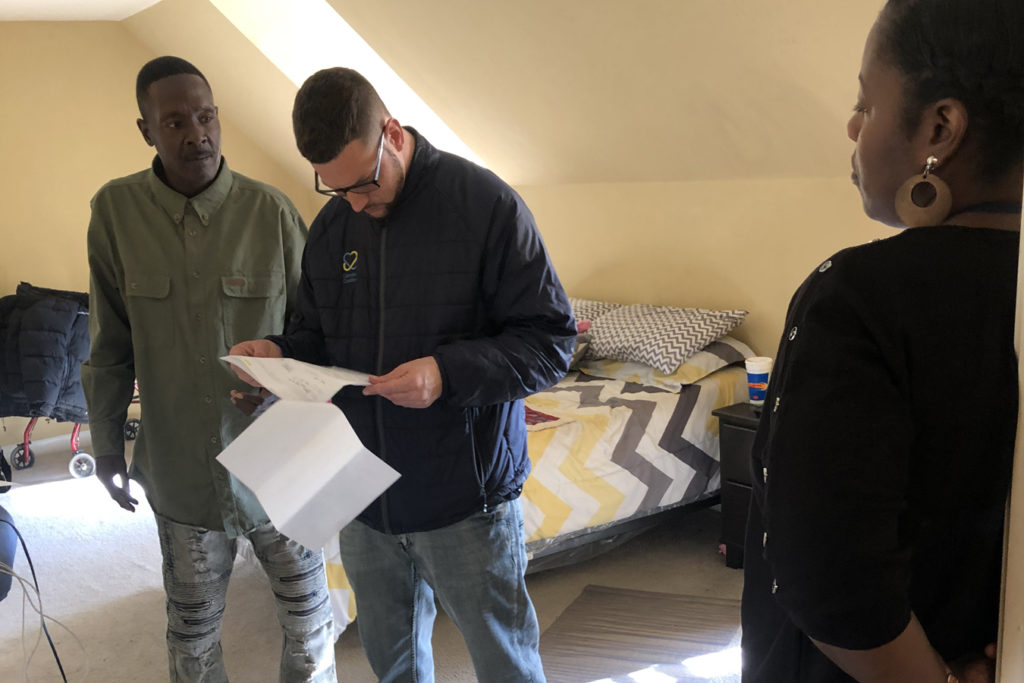
The Camden Coalition helped Moore get an condominium. (Dan Gorenstein/Tradeoffs)
Moore says it took him a month to sleep in his mattress, after years of intermittent homelessness.(Dan Gorenstein/Tradeoffs)
‘I Kid You Not’
“I would have never imagined this,” mentioned Moore, sweeping his arm round his one-bedroom condominium.
A inexperienced houseplant sits within the sunshine. A fluorescent-colored stuffed animal decorates the mattress.
“When I first moved in here,” Moore defined, “it took me about a month to even sleep in my bed. I slept on a couch.”
Housing made it simpler to face his different drawback, selecting to attempt the drug naltrexone, a long-acting injection to deal with alcohol habit.
Moore is sort of two years sober in the present day. He meets with a coalition assist group on Wednesdays. He’s turning into a deacon at his church. In the 22 months he has lived within the condominium, Moore’s journeys to the hospital have plummeted: only one admission and one ER go to.
“I kid you not, when I saw Mr. Moore probably a month ago, I was standing next to him and did not recognize him,” mentioned nurse Skinner. “He looked at me, and said, ‘Jeneen, it’s me. And I was like, ‘My God, you look amazing!’”
Larry Moore’s story is simply that: one story.
Yet it represents a bigger pattern. Insurers — together with UnitedHealthcare underneath Brenner’s course — hospitals and plenty of state Medicaid companies have begun spending thousands and thousands to satisfy sufferers’ social wants.
The new examine, although, backs up the skepticism of different researchers that, on the subject of saving cash not less than, these approaches don’t work properly. For one, applications are costly and exhausting to scale. The coalition’s housing effort presently serves solely 50 folks and prices about $14,000 per individual per yr. Secondly, the information is missing, cautioned Boston University economist Austin Frakt. “Despite what people would like to believe, there’s not a lot of evidence you can reduce health spending by spending more in other areas.”
Finkelstein mentioned that as well being care corporations transfer additional past the 4 partitions of a hospital, the necessity for rigorous analysis grows. “I think a lot of well-intentioned people in health care can’t handle the truth,” she mentioned. “They’re trying to do good, but they don’t have the courage to say, ‘Let’s do a gut check on ourselves.’”
Dan Gorenstein is the creator and co-host of Tradeoffs podcast and Leslie Walker is a producer on the present, which options the examine on the Camden Coalition in episode 7.