The restricted provide of ventilators is among the chief considerations going through hospitals as they put together for extra COVID-19 instances. In Italy, the place hospitals have been overwhelmed with sufferers in respiratory failure, medical doctors have needed to make tough life-or-death selections about who will get a ventilator and who doesn’t.
In the U.S., emergency plans developed by states for a scarcity of ventilators embody utilizing optimistic airway strain machines — like these used to deal with sleep apnea — to assist hospitalized folks with much less extreme respiration points.
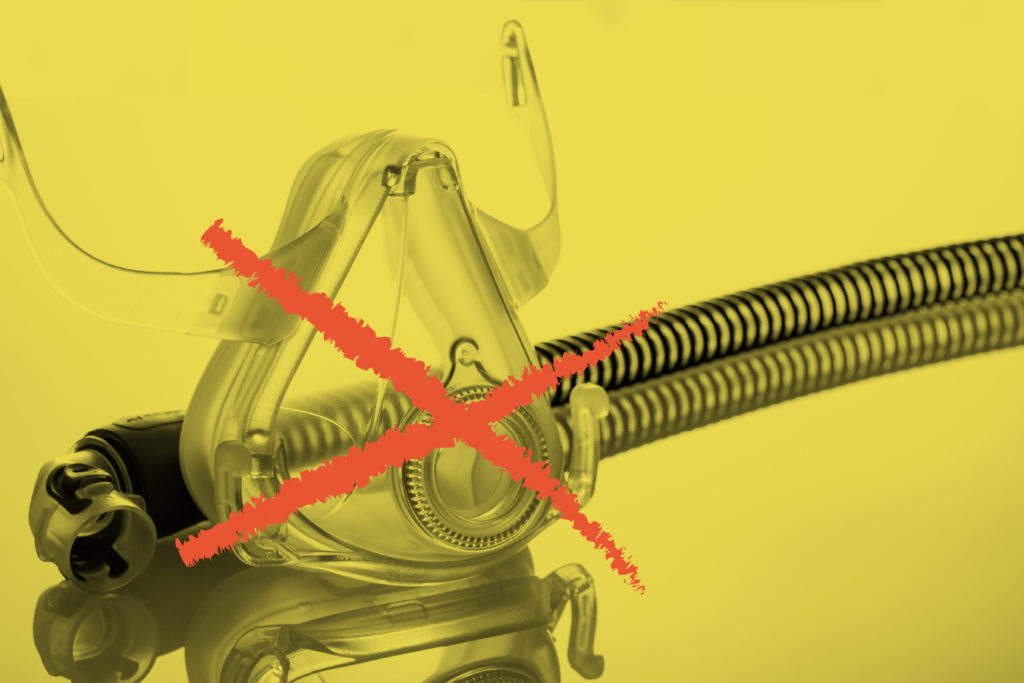
While that measure may stretch the provision of ventilators and save lives, it has a serious disadvantage. Officials and scientists have identified for years that when used with a face masks such various units can presumably enhance the unfold of infectious illness by aerosolizing the virus, whether or not used within the hospital or at residence.
Indeed, that very state of affairs might have contributed to the unfold of COVID-19 inside a Washington state nursing residence that grew to become floor zero within the United States early on. First responders known as to the Life Care Center of Kirkland starting Feb. 24 initially used steady optimistic airway strain machines, usually referred to as CPAPs, to deal with residents earlier than it was identified the sufferers have been contaminated with the COVID-19 virus.
“It’s best practice for us for people with respiratory illnesses,” mentioned Jim Whitney, medical providers administrator for the Redmond Fire Department, whose crews responded to the nursing residence’s 911 calls. “We had no idea that we potentially had COVID patients there.”
It was solely later that King County public well being officers suggested Redmond Fire and different first responders within the area to not use these machines for sufferers suspected of getting COVID-19 sickness. Whitney mentioned responders have been utilizing the machines with specialised filters, which might cut back the quantity of virus launched. But county public well being authorities advocate that first responders keep away from utilizing CPAP altogether. Redmond Fire has now discontinued the usage of CPAPs for COVID-19 sufferers.
“It’s truly out of an abundance of caution for our people and for the community that we put it on the back shelf, unless we can confirm it was the best use for our patient,” Whitney mentioned.
The misstep represents a basic instance of how the well being care system is taking part in catch-up in its effort to cope with the quickly escalating pandemic, and the way essential details about combating the novel coronavirus could be sluggish to achieve these on the entrance traces.
The American Society of Anesthesiologists issued guidance on Feb. 23 discouraging CPAP use in COVID-19 sufferers — recommendation largely knowledgeable by expertise with the SARS epidemic in 2003. Studies courting to 2003 recommend such units can pump viruses into the air, probably rising the unfold of a contagious illness.
During the SARS outbreak in Toronto, half of all SARS instances, together with three deaths, occurred amongst well being care employees. Some of the best threat arose when medical doctors and nurses have been uncovered to aerosolized virus by means of the usage of optimistic airway strain machines or different respiratory remedy units.
The experiences from the Life Care Center of Kirkland now have medical doctors rethinking their methods when confronted with ventilator shortages and their recommendation to first responders about utilizing CPAP machines within the subject.
“In general, we’re just telling them not to use it,” mentioned Dr. Comilla Sasson, an affiliate medical professor of emergency drugs on the University of Colorado School of Medicine. “Because we are concerned about community spread, and we have to assume that anybody with respiratory distress is a COVID patient.”
And medical doctors even recommend those that use the units at residence ought to take precautions to stop infecting others.
How CPAPs Spread The Coronavirus
Ventilators are machines that push air into and out of the lungs by means of tubes inserted down sufferers’ airways once they have hassle respiration on their very own. The machines permit well being care suppliers to fine-tune the quantity of air equipped, the speed of respiration, the quantity of oxygen and the strain as wanted.
Both hospital and residential variations of optimistic airway strain machines are a lot easier units that use excessive strain to push air into the airway, usually by means of a face masks. CPAPs present a steady circulate of air at a relentless strain. More superior bilevel variations, known as BiPAPs, which can be utilized at residence or in well being care amenities, push the air in, however then decrease the strain to permit the air to be exhaled.
“You can actually function certain BiPAP machines to run like ventilators,” mentioned Dr. James Finigan, a pulmonology and significant care specialist at National Jewish Health in Denver.
The key situation, Finigan mentioned, is how the gadget connects to the affected person. Ventilators require a respiration tube and function as closed techniques with a filter that traps any pathogens. Face masks usually used on CPAPs or BiPAPs permit air to flee, pumping the virus into the environment and probably infecting different sufferers, caregivers or anybody close by.
Positive airway strain machines are sometimes step one in the usual algorithm for hospital or emergency personnel when treating folks with sure respiration issues. Finigan mentioned that, in sufferers with commonplace respiratory failure, medical doctors would possibly first see if sufferers can get by on high-flow nasal oxygen or on BiPAP machines to keep away from intubation and sedation.
“If your hope is that maybe this might be a temporizing measure that might hold them from hours to a couple of days, you’ll try to use the mask,” Finigan mentioned. “There are some situations where somebody is breathing OK but is just having trouble getting enough oxygen. Theoretically, a CPAP might be enough to get them enough oxygen. But, again, doing it with a mask is more likely to generate an aerosol and create an infectious problem.”
Dr. Jeff Sippel, a essential care specialist at UCHealth, based mostly in Aurora, Colorado, mentioned BiPAPs could possibly be used for COVID-19 in a closed system with out a masks if sufferers are first fitted with a respiration tube.
“The hardware actually fits,” he mentioned.
The jury-rigged units may then be used for much less extreme COVID-19 sufferers, in addition to for different sufferers who won’t be first in line for a ventilator. More extreme instances would nonetheless require full mechanical respiration like that offered by a ventilator, and it’s unlikely that BiPAP may totally make up for the undersupply of ventilators in a full-blown pandemic.
Some medical doctors have steered that governors ought to put out a name for folks with spare BiPAP machines of their houses to donate them to hospitals. But Sippel mentioned hospitals produce other steps they might take first.
Doctors are investigating whether or not they can join a number of sufferers’ respiration tubes to a single ventilator. At UCHealth, for instance, the hospitals have near 700 ventilators, Sippel mentioned, and will probably use roughly a fifth to ventilate two folks on the similar time.
This week, the Food and Drug Administration offered guidance that enables hospitals to switch respiratory units, together with ventilators, CPAPs and BiPAPs, through the public well being emergency, so long as they take steps to stop aerosolization of the virus.
What About CPAPs For Home Use?
Dr. Christopher Winter, a sleep drugs specialist in Charlottesville, Virginia, mentioned individuals who depend on CPAP machines for sleep apnea can proceed to make use of them so long as they haven’t any signs of COVID-19. But they need to converse to their physicians in the event that they develop upper-respiratory signs, to assist decide if they need to proceed.
Winter is engaged on a information with — and for — different clinicians to assist them determine when sufferers contaminated with the COVID-19 virus ought to preserve utilizing their CPAP machines.
“When does the balance of shooting it all through your house outweigh the negatives to the individual by not using it?” Winter requested.
Anybody who makes use of a CPAP machine at residence, he mentioned, might wish to sleep in a separate room from family members to keep away from infecting them. That’s true even when the particular person with apnea doesn’t have any COVID-19 signs. And if sufferers are suggested by their medical doctors to cease utilizing their machines, Winter mentioned, they need to additionally keep away from driving, as a result of they might be sleep-deprived.
In most components of the U.S., the necessity for additional respiration units in well being care amenities will not be but essential. But hospitals are bracing for a surge in sufferers who will want respiratory help.
“This is getting real now,” mentioned Dr. Matthew Wynia, an internist and bioethicist who has been engaged on UCHealth’s COVID-19 plans. “We are about to be slammed.”