Rachana Pradhan and Samantha Liss
Senators have launched an inquiry into corporations paid billions in taxpayer {dollars} to construct eligibility methods for Medicaid, expressing concern that error-riddled know-how and looming work necessities “will cause Americans to lose Medicaid coverage to this bureaucratic maze.”
The letters, dated Oct. 10, have been despatched to 4 corporations and observe a KFF Health News investigation that uncovered widespread points in states utilizing Deloitte-run methods to evaluate Medicaid eligibility for hundreds of thousands of individuals. Failures have resulted within the inaccurate lack of well being protection and different important safety-net advantages for low-income folks. Malfunctions in these methods can cost millions and take years to repair.
As most states put together to institute work necessities mandated by the tax and home spending regulation President Donald Trump signed in July, senators wrote it’s every firm’s accountability to construct functioning methods, “rather than to prioritize their bottom line.”
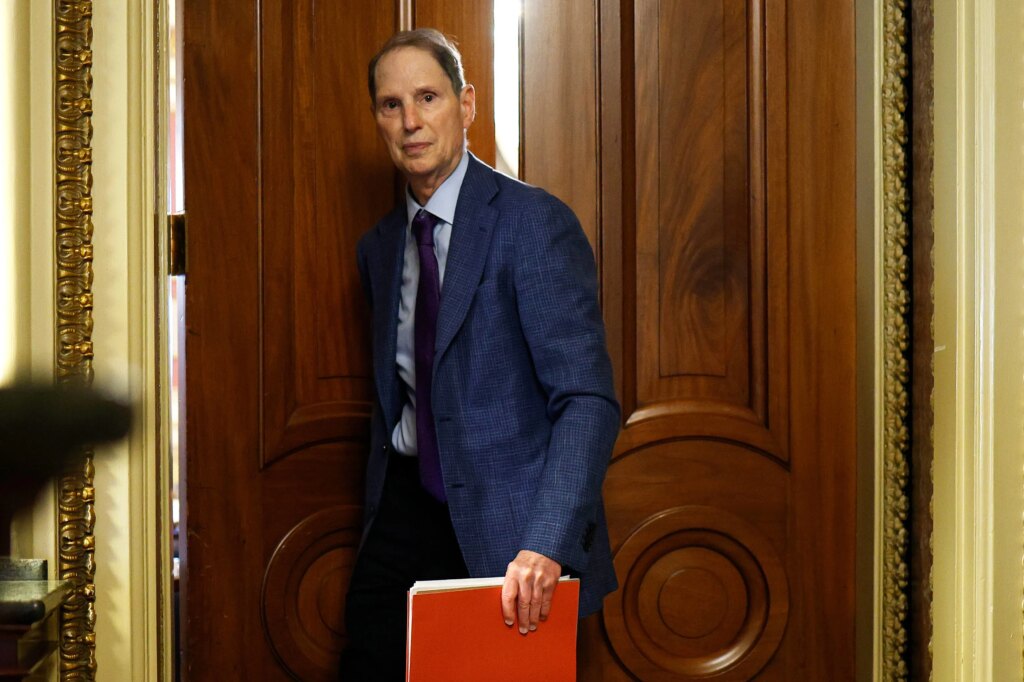
Democratic senators Ron Wyden of Oregon, Elizabeth Warren of Massachusetts, and Raphael Warnock of Georgia, in addition to Sen. Bernie Sanders (I-Vt.), despatched the letters to a number of corporations the Centers for Medicare & Medicaid Services recognized as eligibility system contractors: Deloitte, GDIT, Gainwell Technologies, and Conduent.
“They’re essentially health care middlemen that are in the business of red tape, and they profit when Americans don’t get health care,” Wyden, the highest Democrat on the Senate Finance Committee, which oversees Medicaid, stated in an interview.
“They’ve got a history of poor performance when it comes to determining eligibility or in helping Americans enroll in Medicaid,” Wyden stated. “Without stronger oversight and real accountability, these contractors are just going to get a jumbo windfall for creating systems that actually harm Americans trying to get health care.”
Spokespeople for the 4 corporations didn’t present feedback for this text.
As of June, 70.5 million people have been enrolled in Medicaid, based on CMS.
A handful of states function their very own Medicaid eligibility and enrollment methods, however most depend on contractors to construct and run them. KFF Health News discovered that Deloitte, a world consultancy that generated $70.5 billion in revenue in fiscal yr 2025, dominates this slice of presidency enterprise. Twenty-five states have awarded Deloitte contracts for eligibility methods. The agreements, by which the corporate commits to design, develop, implement, or function state-owned methods, are value at the very least $6 billion, dwarfing any of its rivals.
Kinda Serafi, a associate at Manatt Health, is advising states on the way to reconfigure their methods to include work necessities.
States are in a “major sprint” to make adjustments by 2027, she stated, they usually’re being “inundated” with pitches from distributors seeking to safe contracts. It underscores the enterprise alternative these system adjustments characterize for contractors.
“I think we have to really be vigilant to make sure that these vendors are implementing the requirements consistent with the law,” Serafi stated.
Companies signal contracts with state governments, however the federal authorities pays the majority of the price. The federal authorities covers 90% of states’ prices to develop and implement state Medicaid eligibility methods and 75% of ongoing upkeep and operations bills, based on federal rules.
The Senate letters cite issues with Deloitte-run eligibility methods that KFF Health News recognized. Among different points, the Florida eligibility system erroneously cut benefits for brand new mothers, and an issue in Kentucky prevented protection purposes from getting via on-line, which price $522,455 and took 10 months to resolve.
“Unfortunately, these are just a few examples of third-party systems’ failure to serve their very function: to reliably and accurately determine an individual’s eligibility for Medicaid coverage and services,” the senators wrote.
The senators requested the businesses to reply by Oct. 31 to their questions, comparable to whether or not corporations’ contracts with states embody monetary incentives tying fee to the removing of Medicaid enrollees and whether or not the businesses are penalized for protection terminations made in error. The senators additionally demanded an accounting of the corporate’s lobbying expenditures for the previous 5 years and protocols for making system adjustments.
By 2027, the Congressional Budget Office projected, based mostly on an early model of the invoice, 18.5 million Medicaid beneficiaries should work or full different qualifying actions for 80 hours a month to maintain their advantages, until they qualify for an exemption. The CBO estimates that 5.3 million enrollees will lose protection by 2034.
The new work necessities are simply certainly one of a number of federally mandated Medicaid adjustments which can be forcing states to adapt their eligibility methods.
Medicaid work necessities have been plagued with issues within the few states the place they’ve been examined. Medicaid enrollees have been pissed off in attempting to navigate byzantine guidelines and glitchy know-how. Work necessities have additionally come at nice price.
Georgia has not adopted the ACA Medicaid growth, which has granted advantages to hundreds of thousands of adults incomes as much as 138% of the federal poverty degree. Instead, the state affords advantages to some folks incomes as much as the poverty line who can show they’re working or collaborating in related actions for 80 hours a month. Nearly 110,000 Georgians had utilized to the state’s Georgia Pathways to Coverage program via May, however solely 9,157 folks have been enrolled as of mid-August. Under typical ACA growth guidelines, 336,000 adults would be eligible for protection, based on KFF.
The Georgia program has price $109 million, with $34 million spent on well being advantages and greater than $20 million allotted to advertising and marketing contracts, based on a KFF Health News evaluation of state stories. Deloitte constructed Georgia’s eligibility system and is the first marketing consultant for the Pathways program.
Before Medicaid work necessities turned federal regulation, Arizona additionally submitted a request to federal regulators to launch its personal model that might apply to roughly 190,000 folks.
The state’s utility offered perception into the forms of system adjustments states might quickly must make to handle the brand new federal work requirement.
Arizona Medicaid officers stated they’d collect data on enrollees’ work hours, coaching, and schooling. The state’s eligibility system, which is operated by Accenture, would additionally must examine whether or not somebody is exempt.
States are within the early phases of figuring out adjustments they should make to implement work necessities.
Tessa Outhyse, a spokesperson for the California Department of Health Care Services, stated the state expects upgrades to be processed “through the existing contractual change order process.” State contracts with eligibility corporations usually put aside hundreds of thousands to cowl the price of adjustments, however methods might require upgrades past the agreed-upon work.
In Missouri, upgrades are anticipated to price roughly $33 million, based on a state budget document.
The state has a contract with non-public firm RedMane to deal with a few of its Medicaid eligibility processing. Missouri plans to rent an extra contractor to make sure it correctly institutes Medicaid work necessities, based on Baylee Watts, a spokesperson for Missouri’s Department of Social Services.
Medicaid eligibility contractors “have a lot of leverage and expertise to influence contracts, to win contracts,” Wyden stated. “They can do a lot more, to the value of what we’re giving them.”
KFF Health News senior correspondent Renuka Rayasam and correspondent Sam Whitehead contributed to this report.