This story is a part of a partnership that features WHYY, NPR and Kaiser Health News.
This story could be republished at no cost (details).
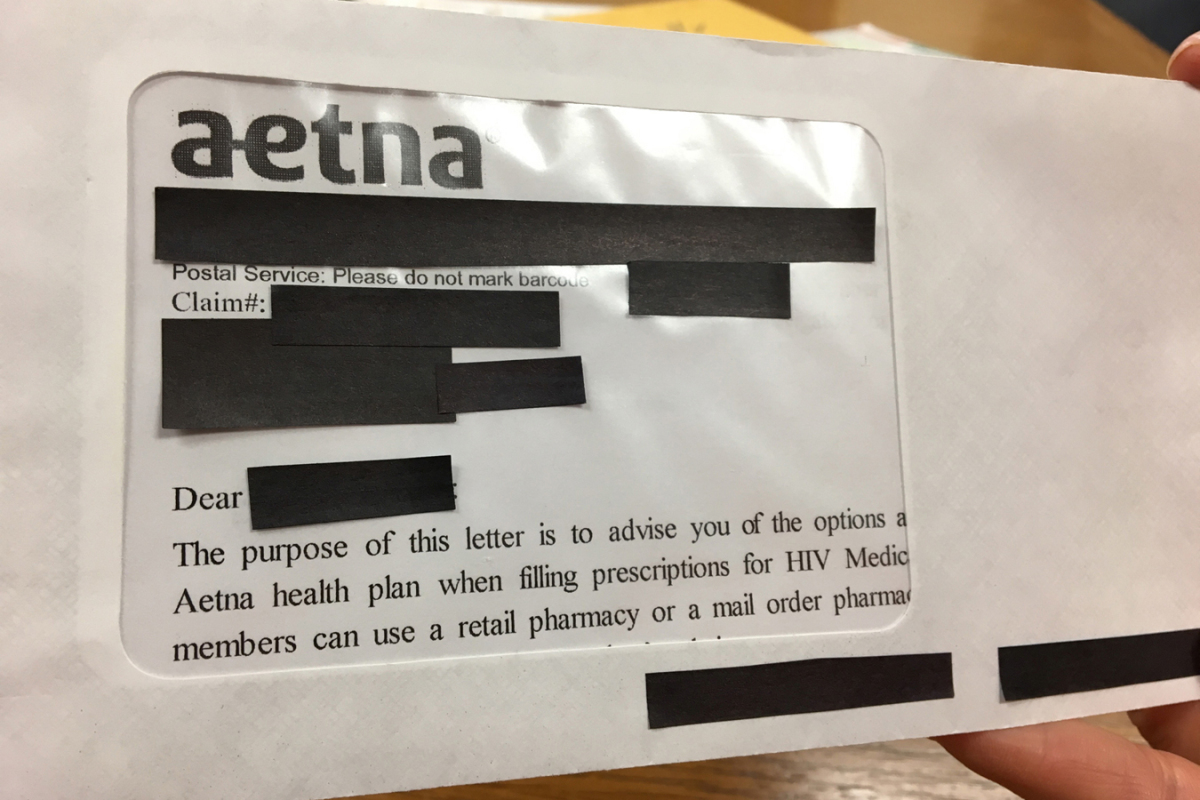
Aetna settled a lawsuit for $17 million Wednesday over an information breach that occurred in the summertime of 2017. The privateness of as many as 12,000 individuals insured by Aetna was compromised in a really low-tech manner: The indisputable fact that they’d been taking HIV medicine was revealed by means of the clear window of the envelope.
“I was shocked,” stated Sam, who distinctly remembers the day he acquired the discover in August. (Kaiser Health News and NPR agreed to not use his full identify as a result of he worries about how going public along with his HIV standing may have an effect on his work.) The letter got here to his mailbox in an condominium advanced in New Jersey. He wasn’t immediately concerned within the lawsuit however says the letter hit a stage of vulnerability he had by no means felt earlier than.
“I haven’t disclosed my HIV status to my parents,” stated Sam, 36, who’s a civil rights lawyer. “Let’s say that letter had gotten forwarded to their house and someone happened to open the mail. Those were the types of things going through my mind.”
In an announcement, Aetna wrote: “Through our outreach efforts, immediate relief program and this settlement we have worked to address the potential impact to members following this unfortunate incident.”
The insurer additionally stated it’s “implementing measures designed to ensure something like this does not happen again as part of our commitment to best practices in protecting sensitive health information.”
Email Sign-Up
Subscribe to KHN’s free Morning Briefing.
In an ironic twist, the letters have been despatched in response to a settlement over earlier privateness violation considerations. Aetna had required members to acquire HIV drugs by means of mail-order pharmacies. The affected individuals had taken treatment to deal with HIV or to decrease the chance of turning into contaminated with the virus, an strategy known as PrEP, or pre-exposure prophylaxis.
Lawsuits filed in 2014 and 2015 alleged that coverage was discriminatory, that it prevented sufferers taking HIV drugs from receiving in-person counseling from a pharmacist and that it jeopardized members’ privateness.
Aetna settled with the person plaintiffs, modified its coverage to permit members to fill HIV prescriptions in individual at retail pharmacies, and, in flip, despatched out notification letters to anybody who had stuffed prescriptions for HIV drugs.
It was these notification letters that contained a big envelope window that uncovered delicate HIV info.
While the stigma surrounding HIV could also be much less extreme than it was and coverings have improved enormously, Ronda Goldfein, director of the AIDS Law Project of Pennsylvania, stated the truth is that critical discrimination nonetheless exists. That means defending affected person confidentiality is crucial to making sure individuals really feel protected getting care.
As lots of of calls from individuals who acquired the Aetna letter began coming into Goldfein’s workplace and others across the nation, she realized of extra harrowing and devastating experiences. She stated she heard from one man who had homophobic slurs painted on his door when neighbors noticed the letter. Other letter recipients felt the necessity to transfer out of their neighborhoods. For one girl, whose standing turned recognized in her tight-knit immigrant neighborhood, “she stopped being able to function, she stopped being able to go to work, and she lost her job,” Goldfein stated.
Adrian Lowe (left), employees lawyer with the AIDS Law Project of Pennsylvania, and Ronda Goldfein, an lawyer and govt director of the AIDS Law Project, filed a class-action go well with towards Aetna over privateness breaches. (Elana Gordon/WHYY)
The AIDS Law Project of Pennsylvania and the Legal Action Center initially issued a requirement letter in late August that the insurer cease the mailings. The firm responded, establishing a aid fund for affected individuals and apologizing. “This type of mistake is unacceptable, and we are undertaking a full review of our processes to ensure something like this never happens again,” the well being insurer stated.
Goldfein and others soon discovered that the mailing was more widespread than first thought: Up to 12,000 individuals had acquired it. Her company, the Legal Action Center and Berger & Montague PC filed a lawsuit and sought class-action status.
The privateness breach as outlined within the proposed settlement was twofold: Aetna launched the names of 13,480 individuals to its authorized counsel and a vendor with out correct authorization. Of these, 11,875 received the letter that exposed they have been taking HIV treatment.
The proposed settlement is awaiting approval in federal courtroom, however in it Aetna has agreed to pay $17 million and arrange new “best practices” to stop one thing like this from occurring once more.
As a part of the payout, the regulation corporations are setting apart a minimum of $12 million for funds of a minimum of $500 to the estimated 11,875 individuals who could have acquired a letter exposing that info, acknowledging that “the harm was in the status being disclosed,” Goldfein stated. Plus, individuals gained’t need to file further paperwork and undergo extra mailings pertaining to their HIV drugs.
A fund can be arrange for individuals who skilled further monetary or emotional misery. Individuals will be capable to declare as much as $20,000. The remainder of the cash will go towards authorized charges and prices.
“It’s a much bigger settlement than ordinary identity theft scenarios, where an online database has been breached and the main injury people are claiming is that they might be victims of identity theft and maybe have their financial information compromised,” stated William McGeveran, a specialist in privateness regulation and knowledge breaches on the University of Minnesota.
The quantity could also be uncommon, however McGeveran additionally stated low-level breaches like this aren’t. Companies could also be so centered on IT safety that they overlook different ways in which privateness could be breached.
“They’re more common than people realize,” McGeveran stated. “There’s so much attention to cybersecurity, and rightly so, but a lot of medical privacy concerns are much more analog than that. They’re about things being overheard, they’re about paper records and in this case it’s about a paper mailing.”
Beyond the payout itself, she hopes the go well with helps change the tradition of corporations in relation to the eye paid to medical privateness, and the rights of individuals with HIV specifically. To spotlight that, attorneys used “Andrew Beckett” because the pseudonym for the unique plaintiff within the case, a Pennsylvania man from Bucks County.
It’s a nod to the Tom Hanks character within the 1993 movie “Philadelphia,” who was fired after his regulation agency discovered he had HIV. This “Beckett” is taking PrEP.
“HIV still has a negative stigma associated with it, and I am pleased that this encouraging agreement with Aetna shows that HIV-related information warrants special care,” the person generally known as Beckett stated in assertion.
This story is a part of a partnership that features WHYY, NPR and Kaiser Health News.
Related Topics Courts Health Industry HIV/AIDS Insurers Privacy