This story additionally ran on USA Today. This story will be republished totally free (details).
The newest miracle machine in fashionable medication — whose use has skyrocketed lately — is saving folks from the brink of dying: adults whose lungs have been ravaged by the flu; a trucker who was trapped underwater in a crash; a person whose coronary heart had stopped working for an astonishing seven hours.
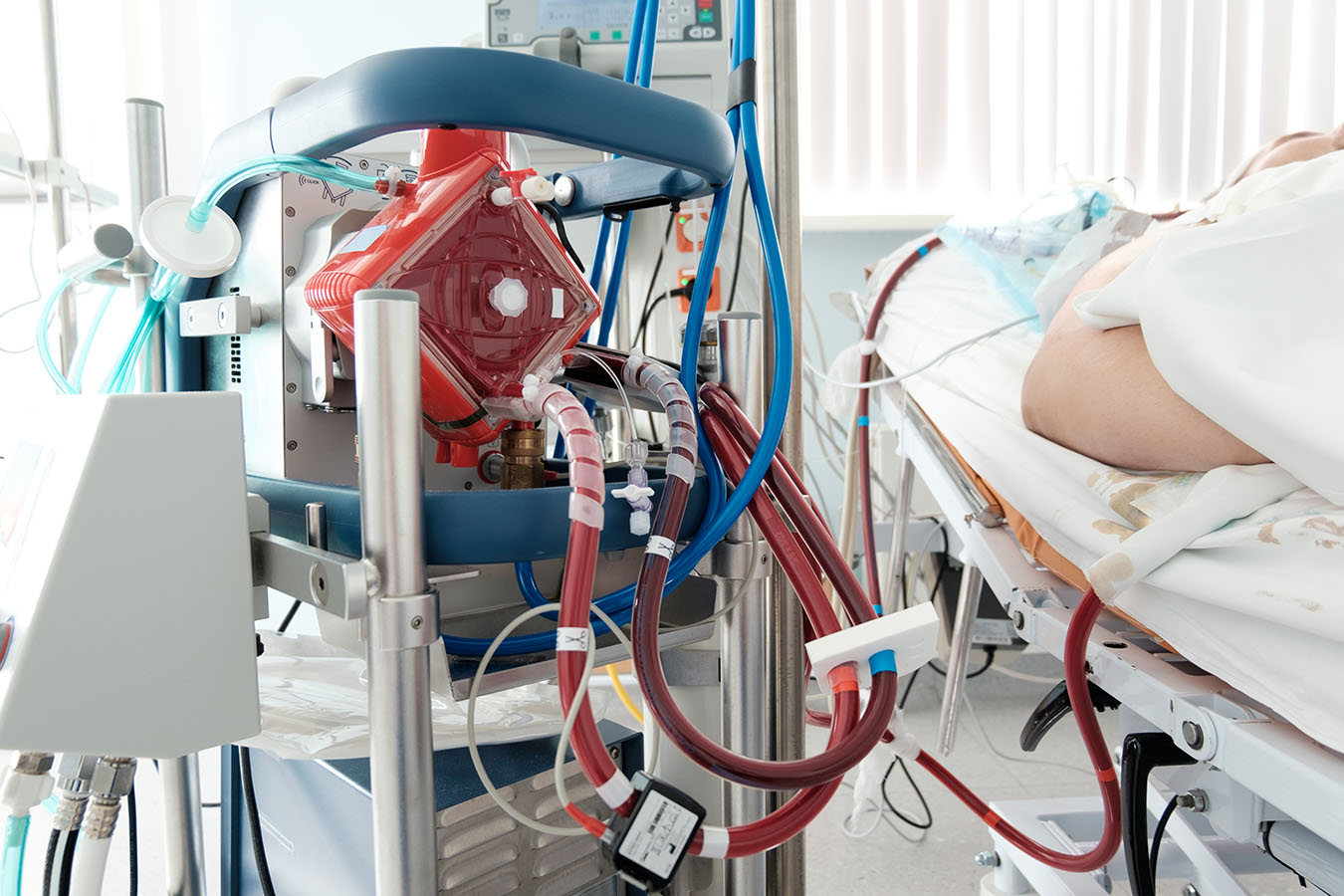
But for every grownup saved by this machine — dubbed ECMO, for extracorporeal membrane oxygenation — one other grownup hooked as much as the tools dies within the hospital. For these sufferers, the intervention is a really costly, labor-intensive and unsuccessful effort to cheat dying.
ECMO, essentially the most aggressive type of life help out there, pumps blood out of the physique, oxygenates it and returns it to the physique, maintaining an individual alive for days, weeks or months, even when their coronary heart or lungs don’t work.
The invention is creating “an entirely new paradigm,” stated Dr. Kenneth Prager, director of medical ethics at Columbia University Irving Medical Center. “You have a heart that’s not working, yet the patient is not dead.”
Most generally used for newborns, ECMO use has been growing dramatically among adults. In the United States, procedures tripled from 2008 to 2014, as much as an estimated 6,890, in line with the federal Agency for Healthcare Research and Quality.
Experts warning that as ECMO turns into extra out there, it’s also getting used as a last-ditch try to purchase extra time for dying sufferers with poor probabilities of survival.
ECMO will not be designed to be a vacation spot, however a bridge to someplace — restoration, transplantation or an implanted coronary heart gadget. But when sufferers are too sick to succeed in these objectives, ECMO can turn out to be a “bridge to nowhere,” leaving the affected person in limbo, probably even awake and alert, however with no probability of survival exterior the intensive care unit. Medical groups and households will be fiercely divided over when to drag the plug.
ECMO may be very costly, principally because of the labor concerned: An individual on ECMO can not reside exterior the ICU and should be repeatedly monitored for problems, reminiscent of blood clots, bleeding, an infection and lack of blood to the limbs. Median prices for ECMO in 2014 had been $550,000, making it the 15th-most-costly process that yr, in line with the AHRQ.
In one latest case, a instructing hospital charged $four.2 million for a 60-day ECMO keep for a 19-year-old man with acute respiratory misery syndrome who was comatose the complete time and didn’t survive, in line with Dr. Merrit Quarum, CEO and founding father of WellRithms, a cost-containment firm. Quarum stated a self-insured well being plan is protecting the invoice.
The variety of U.S. hospitals providing ECMO has greater than doubled from 108 in 2008 to 264 immediately, in line with a registry run by the Extracorporeal Life Support Organization (ELSO), which tracks most however not all packages.
“In the United States, the competition between hospitals is so intense that every hospital wants the ability to provide this level of care,” stated Randy Bartilson, president of the ECMO Advantage consulting agency.
But “as ECMO expands, there’s still a lot of places that still don’t fully understand what it can do and how to use it,” he stated.
Four affected person tales spotlight the promise — and complexities — of this game-changing expertise.
The Seven-Hour Code
Dr. Jessica Zitter was working within the ICU in an Oakland, Calif., hospital someday when she acquired summoned for a code blue. A 60-year-old affected person had arrived with a coronary heart assault. His coronary heart went into ventricular fibrillation, the place it simply wiggled like “a bag of worms,” she stated.
Hospital workers began pumping their palms on the person’s chest and put a tube in his throat to assist him breathe. Every so typically, they stood again and zapped his coronary heart with an electrical shock. It didn’t work. So, they strapped onto his chest a LUCAS machine, which robotically performs chest compressions like a jackhammer.
The man’s oxygen ranges had been plummeting. At the identical time, Zitter recalled, he stored transferring, giving her the sensation there was a life to be saved. The medical workforce determined to go to the subsequent degree: ECMO. Everyone waited, with the jackhammering compressions nonetheless going, as an ECMO workforce scrambled to get there from one other hospital throughout town.
Zitter watched in awe because the ECMO workforce from the University of California-San Francisco started working. They caught one big tube in a femoral artery and one in a femoral vein. As they pumped his blood out, it was black from deoxygenation. But after it ran by the ECMO machine, she recalled, it remodeled right into a brilliant pink.
(Courtesy of University of Iowa Hospitals & Clinics)
Once on ECMO, the affected person didn’t want his coronary heart, so it may sit idle and get better. Zitter watched as oxygen returned to his physique and mind. He was whisked again to UCSF.
Zitter, who has written concerning the overuse of recent expertise to delay dying, wasn’t optimistic. The affected person had coded, with folks and machines ramming his failing coronary heart, for an astonishing seven hours earlier than ECMO arrived. But as she stored tabs on the affected person, she was amazed to study that he was capable of get better and go house.
The case was a “big shocker,” Zitter stated.
But it was “a crazy, crazy, crazy outlier case with a crazy, crazy, crazy outlier response,” she cautioned. “When these kinds of things happen, people tend to look at them and assume that they will have the same odds. The reality is that they won’t.”
When sufferers obtain ECPR (ECMO for cardiopulmonary resuscitation), solely 29% make it out of the hospital alive, in line with international statistics from ELSO. Survival charges are greater for individuals who use ECMO for under the lungs (59%) or solely the guts (42%), in line with ELSO.
Saving ‘Santa’
A extra frequent final result for ECPR seems one thing like what Dr. Haider Warraich of Duke University Medical Center got here throughout three or 4 years in the past throughout his cardiology coaching.
Warraich was known as to the ready space of a lung transplant clinic, the place a person in his 60s had collapsed on the ground attributable to a coronary heart assault. The man, who had white hair and a scraggly beard, performed Santa each Christmas, Warraich later discovered. “Santa” — as Warraich refers to him in his upcoming ebook, “State of the Heart” — had acquired a brand new set of lungs after his had been wrecked by smoking and lung illness.
The man’s coronary heart, starved of oxygen, sped up right into a malignant rhythm. CPR and electrical shocks didn’t convey it again. Motivated to avoid wasting not solely the affected person however the brand new set of lungs he had acquired, the workforce known as in ECMO.
The ECMO squad arrived with catheters “the size of small javelins,” Warraich recalled. Once Santa was connected on ECMO, the exhausted CPR workforce may cease. Cardiologists did surgical procedure on a blocked artery, however they by no means acquired his coronary heart again to regular. The man lingered for a month, utilizing ECMO for his coronary heart, a ventilator for his lungs and dialysis for his kidneys, earlier than he died.
In this case, utilizing ECMO felt acceptable, Warraich stated. But he stated medical doctors want extra steering to find out which sufferers would profit essentially the most and to stop overuse.
“If you have someone who is dying in front of you, it’s really hard to step back and think about it,” he stated.
The expertise, developed within the 1970s, was initially used primarily for newborns. Early medical trials in adults had been discouraging. But in 2009, the CESAR trial within the United Kingdom confirmed constructive outcomes for ECMO in adults with extreme respiratory failure. Those findings, mixed with improved expertise and an epidemic of swine flu, prompted a swift progress of ECMO amongst adults. The common age for U.S. adults receiving ECMO is 51, one study found. About 1 in 10 ECMO instances are for folks over 65.
Warraich and different specialists say they’re now involved that new organ-donation guidelines might inadvertently spur hospitals to position extra sufferers on ECMO: Under guidelines authorised by the Organ Procurement and Transplantation Network final October, sufferers on ECMO soar to the entrance of the guts transplant ready record.
Email Sign-Up
Subscribe to KHN’s free Morning Briefing.
An ‘Unbearable’ Choice
Once a affected person is on ECMO, deciding when to cease may cause ethical misery and division amongst medical workers, stated Dr. Robert Truog, director of the Center for Bioethics at Harvard Medical School.
In one case Truog described in The Lancet, a 17-year-old boy got here to the ICU at Boston Children’s Hospital, the place Truog works as a doctor. The boy, who had already had one lung transplantation for cystic fibrosis, was now in end-stage respiratory failure. The solely technique to save his life was to present him one other set of lungs. He began on ECMO as a bridge remedy whereas he awaited transplantation.
The boy was absolutely acutely aware, doing homework, texting pals and visiting with household. But after two months of dwelling within the ICU, he was identified with untreatable most cancers that made him ineligible to obtain new lungs.
Clinicians had been deeply divided over what to do subsequent, Truog stated. Some wished to cease ECMO instantly as a result of its unique objective — a bridge to transplantation — was not potential.
Others argued that although he couldn’t survive exterior the ICU, the boy appeared to have a great high quality of life on ECMO, and his household and pals “derived benefits from his continued survival,” Truog wrote. They argued that the household ought to have the proper to proceed this type of life help, simply as with dialysis, air flow or a man-made coronary heart.
A 3rd argument arose, Truog stated: If leaving this affected person on ECMO was acceptable, then in equity “why don’t we put everyone with respiratory failure on ECMO?”
For the dad and mom, Truog stated, it was “unbearable” to decide on a day or second to show off ECMO, as a result of they knew their little one would instantly die.
Clinicians devised an alternate the household would conform to: They determined to not substitute the ECMO oxygenator, a component that must be modified each week or two when it develops blood clots. After a few week, the oxygenator step by step failed and the affected person misplaced consciousness and died, Truog stated.
The resolution “allowed him to die in a way where we didn’t feel like we were choosing the moment of his death,” he stated.
The resolution was not optimum, Truog stated. But “no matter how you do this, it’s going to be very emotionally upsetting to everyone. These are the cases that make some people leave the profession because they’re so hard.”
A Long Goodbye
Karen Ayoub had by no means heard of ECMO till her husband turned direly in poor health.
Philip Ayoub, 58, an accountant and former comptroller for the National Football League, was a “huge personality” and a household man; the couple raised twin boys in Greenwich, Conn. Heart illness, which ran in his household, hit him early: He had his first coronary bypass surgical procedure at age 30 and his second at 43, she stated.
“He knew that his life might be foreshortened” and “tried to pack as much living into it as possible,” stated Karen Ayoub, 55. Her husband instructed her he didn’t need any extraordinary lifesaving measures — he was pleased with the life he had lived, she stated.
In December 2017, he had a 3rd bypass surgical procedure at a hospital on Long Island, and it didn’t go properly. His coronary heart was weaker than anticipated. He turned unconscious, and it wasn’t clear if he would ever get up. He was transferred to Columbia University Irving Medical Center, which has an ECMO program.
Philip Ayoub, 58, an accountant and former comptroller for the National Football League, together with his twin sons. Heart illness, which ran in his household, hit him early: He had his first coronary bypass surgical procedure at age 30 and his second at 43.(Courtesy of Karen Ayoub)
Karen Ayoub stated it was a reasonably simple choice to place her husband on ECMO: “I thought he deserved any chance possible to recover,” she stated. But she didn’t know the way he’d react.
“I wasn’t sure if he was going to wake up and say, ‘Why did you do this? I didn’t want any of this!’” she recalled.
When her husband regained consciousness, he mouthed the phrases: “Why am I here?”
He remained within the ICU for 2 months, on a feeding tube, respiratory tube, ECMO and dialysis. His time there was not simple, she stated: Her husband, who had endured a sequence of mini-strokes in the course of the bypass surgical procedure, started to expertise post-traumatic stress dysfunction, evening terrors and unwanted side effects from medicines.
The solely possibility for additional remedy, she stated, was to get an implanted gadget that may assist his coronary heart pump. But as he weighed that call, and the standard of life he would have, the window of time closed when he was eligible for the gadget, Karen Ayoub stated.
When additional remedy turned out of attain, it was clear her husband was going to die.
“His body was failing him,” Karen Ayoub stated. “It was time.”
She stated the 2 months within the ICU felt like “a gift,” as a result of she and her youngsters acquired to spend additional time together with her husband.
“I’ll always love you, I’ll always be with you,” he instructed his spouse again and again throughout that point.
She stated she would make the identical selection once more to provoke ECMO, however “I don’t know about him — he was the one laying in that bed for two months, being tortured by needles and night visions.”
After they ran out of remedy choices, the household gave permission for the hospital to discontinue life help. Philip wasn’t afraid, she stated: As his remaining day approached, he instructed her, “I can’t wait to see what comes next.”
Philip was sedated earlier than ECMO was turned off. Karen Ayoub laid her head on her husband’s chest and held his palms as he died.
“It was peaceful and respectful,” she stated, “exactly what he wanted.”
‘Futile’ Care
While the Ayoub household bravely accepted their destiny, different households can’t convey themselves to let go, stated Dr. Shunichi Nakagawa, a palliative care physician at Columbia who cared for Philip Ayoub.
Some ECMO sufferers have extreme, irreversible mind injury, can’t take part in decision-making and bear no probability of constructing it out of the hospital alive. For them, ECMO represents “the most extreme form of medical futility,” Nakagawa argued in an article he and Prager co-authored with a colleague within the journal Circulation. They argue that clinicians ought to have the authority to finish or restrict life help in such hopeless instances, even when the household objects.
Whether they will do this depends upon the place they observe: Laws in states reminiscent of Idaho, Oklahoma and New York make it troublesome to withdraw life-sustaining remedy like ECMO with out consent from sufferers or their households, stated Thaddeus Mason Pope, director of the Health Law Institute at Mitchell Hamline School of Law in St. Paul, Minn. But in states like California, Texas and Virginia, clinicians might withdraw ECMO with out consent, he stated.
Dr. Robert Bartlett, a pioneer of the ECMO subject and professor emeritus on the University of Michigan, stated he trains medical doctors that after ECMO turns into a bridge to nowhere, they need to inform the household, “We talked about futility, and now we’re there. So we’re going to turn the circuit off tomorrow.”
“It’s extremely discourteous to the family to ask the family what to do,” he stated.
At Cedars-Sinai Medical Center in Los Angeles — the place sufferers with poor probabilities of survival had been being placed on ECMO, and households had been getting conflicting messages concerning the potential profit — workers launched an improvement effort that has created extra consensus and consistency round acceptable ECMO care, in line with Dr. Michael Nurok, medical director of the cardiac surgical procedure ICU.
At the University of Southern California’s Keck Hospital, each household of an ECMO affected person meets weekly with palliative care and different clinicians to speak about objectives of care — conversations which have been “transformative” for households, stated Dr. Sunita Puri, medical director of palliative medication and supportive care.
In Boston, Dr. Daniela Lamas, a vital care physician at Brigham and Women’s Hospital, stated she has seen ECMO’s promise and its limitations.
“With every escalation and fancy machine comes a lot of hope,” Lamas stated. “It’s really hard to temper that hope with the realities that with each new thing comes a host of ethical questions and dilemmas.”
ECMO, she stated, is “a fantastic example of ‘just because you can, doesn’t mean you should.’”
This story additionally ran on USA Today. This story will be republished totally free (details).
Melissa Bailey: [email protected]”>[email protected], @mmbaily
Related Topics Health Industry Hospitals src=”http://platform.twitter.com/widgets.js” charset=”utf-Eight”>