After a gradual begin, testing for COVID-19 has ramped up in current weeks, with large industrial labs leaping into the trouble, drive-up testing websites established in some locations and new forms of exams accepted beneath emergency guidelines set by the Food and Drug Administration.
But even for people who find themselves capable of get examined (and there’s nonetheless a big lag in testing capability in sizzling spots throughout the U.S.), there generally is a frustratingly lengthy look forward to outcomes — not simply hours, however typically days. Sen. Rand Paul (R-Ky.) didn’t get his optimistic check outcomes for six days and is now being criticized for not self-quarantining throughout that point.
We requested specialists to assist clarify why the turn-around time for outcomes can fluctuate extensively — from hours to days or perhaps a week — and the way that is likely to be altering.
It’s A Multistep Process
First, a pattern is taken from a affected person’s nostril or throat, utilizing a particular swab. That swab goes right into a tube and is shipped to a lab. Some massive hospitals have on-site molecular check labs, however most samples are despatched to exterior labs for processing. More on that later.
That transit time often runs about 24 hours, nevertheless it may very well be longer, relying on how far the hospital is from the processing lab.
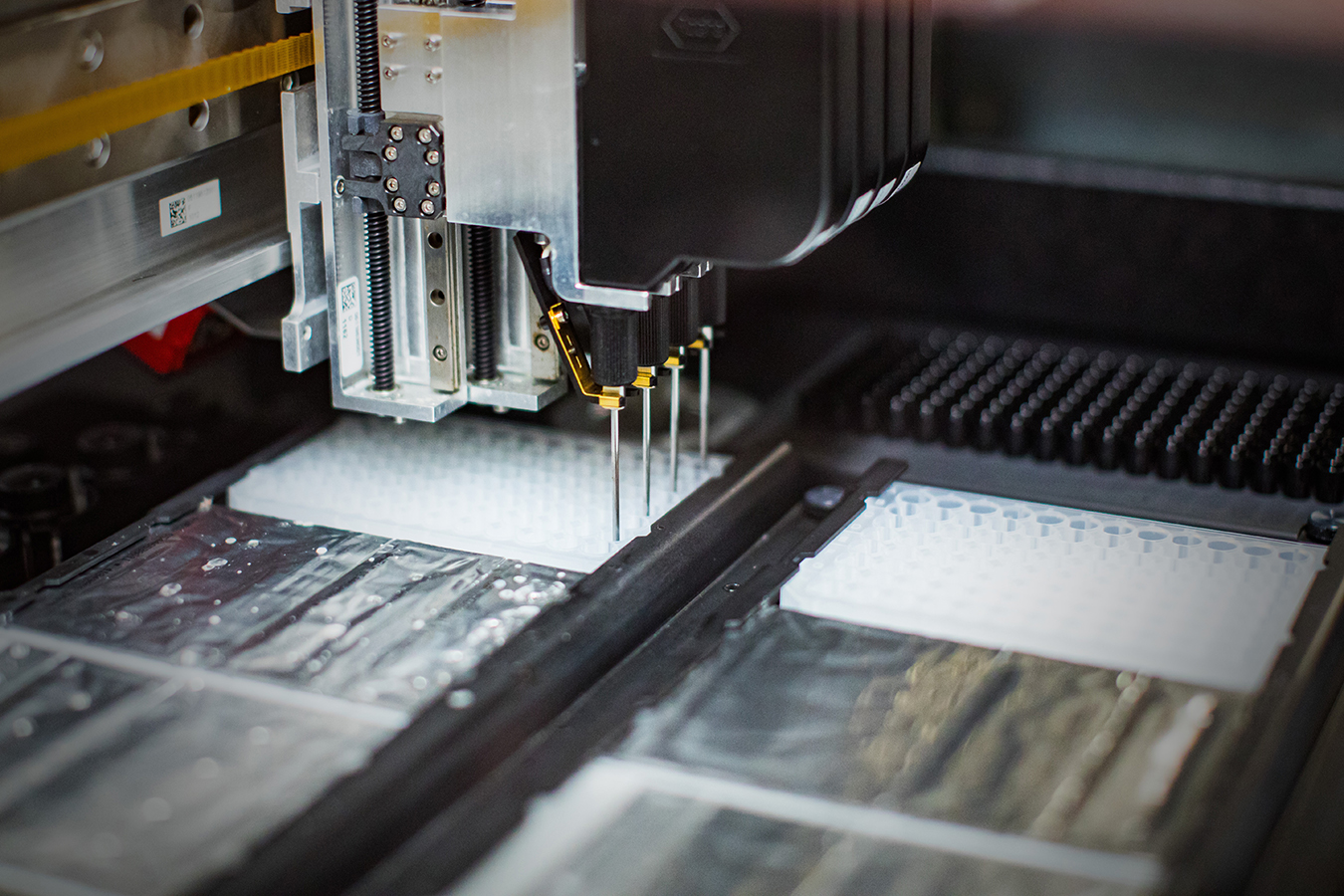
Once on the lab, the specimen is processed, which suggests lab staff extract the virus’s RNA, the molecule that helps regulate genes.
“That step of cleaning, the RNA extraction step, is one limiting factor,” mentioned Cathie Klapperich, vice chair of the division of biomedical engineering at Boston University. “Only the very biggest labs have automated ways of extracting RNA from a sample and doing it quickly.”
After the RNA is extracted, technicians additionally should fastidiously combine particular chemical substances with every pattern and run these mixtures in a machine for evaluation, a course of referred to as polymerase chain response (PCR), which may detect whether or not the pattern is optimistic or unfavorable for COVID.
“Typically, a PCR test takes six hours from start to finish to complete,” mentioned Kelly Wroblewski, director of infectious illness applications on the Association of Public Health Laboratories.
Some labs have bigger staffs and extra machines, to allow them to course of extra exams at a time than others. But even for these labs, as demand grows, so does the backlog.
Capacity Is Expanding, But Not Enough
Initially, only some public well being labs and the federal Centers for Disease Control and Prevention processed COVID-19 exams. Problems with the primary CDC check kits additionally led to delays.
Now the CDC has a greater package, and 94 public well being labs throughout the nation do COVID-19 testing, mentioned Wroblewski.
But these labs can’t probably do all that’s wanted. In regular occasions, their essential operate is common public well being surveillance — detecting extra widespread threats equivalent to outbreaks of measles or monitoring seasonal influenza — “but not to do diagnostic testing of the magnitude that is required in this response,” she mentioned.
Large industrial labs like these run by corporations equivalent to Quest Diagnostics and LabCorp got the go-ahead late final month by the FDA to begin testing, too.
The FDA has mentioned it gained’t cease sure personal labs — these which can be already licensed to carry out complicated testing — and diagnostic corporations from growing their very own check kits. Labs at some big-name hospital programs, equivalent to Advent Health, the Cleveland Clinic and the University of Washington, are amongst these doing this.
In addition, the FDA has accepted greater than a dozen testing kits by numerous producers or labs beneath particular emergency rules designed to hurry the method. Those embody exams by Quest Diagnostics, LabCorp, Roche, Quidel Corp. and others. The kits are utilized in PCR machines, both in hospital labs or massive industrial labs.
“A chief medical officer on the East Coast said that, up until two days ago, on average it was taking 72 hours to get results,” mentioned Susan Van Meter, government director of AdvaMedDx, a division of the Advanced Medical Technology Association, a tool and diagnostics business commerce group. “That will get better as our member companies come on the market.”
Even so, provide isn’t maintaining with demand, Roche CEO Severin Schwan informed CNBC on March 23. Roche gained the primary approval from the FDA for a check package beneath emergency guidelines, and it has delivered greater than 400,000 kits to date.
“Demand continues to be much higher than supply,” Schwan informed CNBC. “So we are glad that overall capacity is increasing, but the reality is that broad-based testing is not yet possible.”
How Many Tests Can Be Done At A Time?
That varies. Large industrial labs can do so much. LabCorp, for instance, mentioned it’s processing 20,000 exams a day — and hopes to do extra quickly. Other check package makers and labs are additionally ramping up capability.
Smaller labs — equivalent to molecular labs at some hospitals — can do far fewer per day however get outcomes to sufferers sooner as a result of they save on transit time.
Still, it’s often solely massive tutorial medical facilities and a few well being programs which have their very own molecular testing labs, which require complicated tools.
One of these is Medstar Georgetown University Hospital in Washington, D.C.
“From beginning to results can take five to six hours,” mentioned Joeffrey Chahine, technical director for the molecular pathology division there.
Even at such hospitals, the exams are sometimes prioritized for sufferers who’ve been admitted and employees who might need been uncovered to COVID-19, mentioned Chahine. His lab can course of 93 samples at a time and run just a few cycles a day, as much as about 280, he mentioned. Last week, it did 186 a day, three days in a row.
But hospitals with this capability are usually “not testing from their outpatient centers or the ER,” he mentioned. In different phrases, the in-house labs aren’t operating exams from walk-in sufferers.
Those exams are despatched to massive exterior labs “so as not to overwhelm the hospital lab.” While these exterior labs have massive staffs, “the demand is so high that these outpatient clinics and ERs say the turnaround time can be four to seven business days,” he mentioned.
Supply Shortages Are Slowing Test Production
As the worldwide demand for testing has grown, so, too, have shortages of the chemical brokers used within the check kits, the swabs used to get the samples, and the protecting masks and kit utilized by well being staff taking the samples.
“There is an inadequate supply of so many things associated with testing,” mentioned Wroblewski, which is why her group, together with officers in states together with New York and cities together with Los Angeles, advocate prioritizing who ought to be examined for COVID-19.
At the entrance of the road, she mentioned, ought to be well being care staff and first responders; older adults who’ve signs, particularly these dwelling in nursing properties or assisted dwelling residences; and individuals who might produce other diseases that will be handled otherwise in the event that they have been contaminated. Bottom line: prioritizing who’s examined will assist velocity the turnaround time for getting outcomes to folks in these circumstances and cut back their danger of spreading the sickness.
Still, pressing shortages of among the chemical substances wanted to course of the exams are hampering efforts to test health care workers, together with at hospitals equivalent to SUNY Downstate medical heart in hard-hit New York.
Looking ahead, corporations are engaged on faster exams. Indeed, the FDA in current days has approved exams from two corporations that promise leads to 45 minutes or much less. Those can be obtainable solely in hospitals which have particular tools to run them. One of these corporations, Cepheid of Sunnyvale, California, says about 5,000 U.S. hospitals have already got the tools wanted to course of these exams. Both companies say they’ll ship to the hospitals quickly however have given few specifics on amount or timing.
But many public well being officers say docs and clinics want a very fast check they will use of their places of work, one just like the exams already in use for influenza or strep throat.
Various corporations are transferring in that course. Late Friday, as an example, Abbott Laboratories announced that the FDA has given emergency-use authorization for the corporate’s fast, point-of-care check, which may ship optimistic leads to as little as 5 minutes and unfavorable leads to 13.
The exams are processed on a small system already put in in 1000’s of medical places of work, ERs, pressing care clinics and different settings. Abbott mentioned it’ll start this week to make 50,000 exams obtainable per day.
“That’s going to make a meaningful difference,” mentioned Van Meter at AdvaMedDx, who believes the fast exams are a vital piece within the continuum of accessible testing.
Even although lab-based PCR exams, that are accomplished at massive labs and tutorial medical facilities, can take a number of hours to supply a end result, the machines used can check excessive numbers of instances unexpectedly. The fast check by Abbott — and different, related exams now beneath improvement — do far fewer at a time however ship outcomes a lot sooner.
“This can be provided in a doctor’s office or an ER, helping to triage patients who are waiting to get in,” mentioned Van Meter. “It’s a very fine complement to the testing that exists.”