Dinah Jimenez assumed a world-class hospital could be higher ready than a chowder home to tell staff once they had been uncovered to a lethal virus.
So, when her boyfriend, an worker of a well-liked seafood restaurant in Seattle, obtained a name from his boss on a Sunday in late March telling him a co-worker had examined optimistic for COVID-19 and that he wanted to quarantine for 14 days, she stated she assumed she’d get an analogous name from the University of Washington Medical Center. After all, the contaminated restaurant worker labored a second job alongside her on the hospital’s Plaza Cafe.
That name by no means got here, she stated.
Jimenez, 42, stated she returned to her job as a cashier on the hospital cafeteria two days later, and “it was like nothing had happened. They didn’t say anything.” She stated the contaminated employee, a fellow cashier, was stationed simply 2 ft from her throughout a typical shift and that neither had been carrying a masks. “He was as close to me as the person sitting behind you in an airplane,” Jimenez stated.
Word slowly unfold among the many cafeteria crew co-worker had the virus, she stated. In the times that adopted, two extra staff fell ailing. But communication in regards to the outbreak was not broadly disseminated by the ranks, in accordance with Jimenez and different staff interviewed. It wasn’t till April, Jimenez stated, that the hospital began offering staff with one masks per day. Just a few weeks later, staff stated, they realized a fourth employees member had examined optimistic for the virus.
From cafeteria employees to docs and nurses, hospital staff across the nation report irritating failures by administration to inform them once they have been uncovered to co-workers or sufferers recognized to be contaminated with COVID-19. Some medical facilities do fastidiously hint the shut contacts of each contaminated affected person and employee, alert them to the publicity and provide steerage on the subsequent steps. Others, by coverage, don’t personally observe up with well being staff who unknowingly handled an contaminated affected person or labored with a colleague who later examined optimistic for the virus.
“It’s an enormous issue,” stated Debbie White, president of the Health Professionals and Allied Employees, a union representing nurses and different well being care professionals in New Jersey. “When a patient is positive, our expectation is that the employer would go back and do their due diligence in terms of investigating who was participating in that patient’s care.”
Instead, she stated, union members typically report “there is very, very little follow-up” to tell them after an publicity.
The disconnect between hospital coverage and employee expectations typically facilities across the lack of clear, direct communication with particular person staff who’ve been doubtlessly uncovered to the coronavirus. And when staff are knowledgeable about an contaminated colleague or affected person, some say that the efforts to hide that individual’s identification could make it tough to gauge the extent of threat.
Melissa Johnson-Camacho, a nurse at UC Davis Medical Center in Sacramento, California, stated she was knowledgeable that one other nurse in her unit examined optimistic, however not which one.
“I don’t know who that nurse is. I don’t know if I had lunch with that nurse. I don’t know if I helped that nurse with a patient,” stated Johnson-Camacho, who’s a chief nurse consultant for the California Nurses Association.
UC Davis Health spokesperson Charles Casey stated federal and state privateness legal guidelines forestall the hospital from figuring out people who check optimistic. HIPAA, the federal privateness rule, does allow some disclosures of private well being info to well being care staff throughout an outbreak of infectious illness, however solely the “minimum necessary,” in accordance with latest steerage from the Office for Civil Rights, which is a part of the U.S. Department of Health and Human Services.
Other hospitals contend that as a result of group transmission of COVID-19 is so widespread, staff ought to assume anybody they encounter, inside or exterior the hospital, could possibly be contaminated and adapt their habits accordingly.
OHSU Health Hillsboro Medical Center, a significant supplier exterior Portland, Oregon, for instance, just lately despatched an e mail to all staff saying that as a result of COVID-19 is widespread in that group, “you will no longer receive notification from [the Employee Health program] after caring for a patient with COVID-19. Instead, we ask that you serve as our eyes and ears and report any concerns for exposure to Employee Health as soon as possible.”
Based on related reasoning, the federal Centers for Disease Control and Prevention issued updated guidelines in April to say hospitals ought to think about forgoing contact tracing for his or her staff — a basic of public well being work that includes figuring out individuals who have been uncovered and asking them to quarantine — in favor of common masking and screening for signs at first of shifts.
While all hospital staff, from meals service to custodial employees, are weak to publicity, nurses and different direct-care suppliers who work together carefully with sufferers are at biggest threat. Informing them of affected person exposures is usually much less necessary in intensive care items and wards designated for COVID-19 assessments, the place sufferers are assumed to have the virus and correct protecting gear needs to be used. But when suppliers take care of a affected person hospitalized for an unrelated situation who later exams optimistic, staff say the data may be essential.
“A lot of nurses are caregivers, too, and we have people at home who are in the high-risk group,” stated Johnson-Camacho, the UC Davis nurse. “No one wants to take this home to their family or someone they love.”
Knowing about an publicity may make the distinction when deciding whether or not to hug your youngsters or transfer out of the household residence, Johnson-Camacho added.
At Stroger Hospital in Chicago, nurse Elizabeth Lalasz stated she contracted the coronavirus after spending a number of hours with a affected person who got here in with what initially was believed to be a continual respiratory situation, however who later was despatched residence with a presumed case of COVID-19. Lalasz stated the hospital by no means adopted up along with her in regards to the presumed publicity, though she had not been carrying correct protecting gear. She stated she subsequently fell ailing and examined optimistic for the virus — and that her co-workers had been by no means knowledgeable about her situation.
“The contact-tracing idea didn’t even exist,” Lalasz stated.
Cook County Health, which operates Stroger, didn’t immediately reply to questions on its insurance policies on informing staff about publicity to the virus. But spokesperson Deborah Song stated the system is following CDC pointers.
At UW Medicine in Seattle, the place the cafeteria outbreak performed out, spokesperson Tina Mankowski stated the hospital isn’t doing contact tracing when staff or sufferers check optimistic for COVID-19. She stated that’s as a result of the medical heart isn’t asking staff to quarantine at residence following a possible publicity.
Under present coverage, if an worker contracts the virus, that individual’s supervisor is notified basically phrases, and is meant to share that info with different employees members. Employees are requested to self-monitor for fever or upper-respiratory signs, and to remain residence if they’re ailing.
Mankowski confirmed that 4 cafeteria staff had examined optimistic for the virus. She stated staff had been notified however didn’t present specifics about how or when.
“The safety of University of Washington Medical Center patients and employees is our top priority,” Mankowski wrote in an e mail. “If an employee tests positive for COVID-19, the manager is informed that one of their employees has tested positive and then discusses this with the staff in that area.”
Jimenez and three different staff stated that was not their expertise and that communication in regards to the outbreak was muted.
Luis Rios, a prepare dinner on the cafeteria for 17 years, stated he was not knowledgeable after the primary colleague examined optimistic, although he had chatted with the sick cashier within the employees locker room a number of occasions, not more than 2 ft away. Just a few days after that employee was recognized, Rios stated, he was taste-testing a dish when he observed his sense of style was dulled, a symptom of COVID-19. He additionally felt chilly, even within the heat kitchen. He was examined at an space medical clinic, and have become the unit’s second confirmed case.
“Honestly, I don’t know if UW or my managers care about workers’ lives,” stated Rios, 49, who spoke by an interpreter. “They only care if we can go in and work.”
Justin Lee, communications director for the Washington Federation of State Employees (WFSE), which represents the cafeteria staff, stated supervisors did submit a replica of an e mail from the worker well being division to cafeteria administrators notifying them basically phrases when the primary employee examined optimistic. A printout was tacked close to the workers’ time clock. But many staff didn’t see it or could have been unable to grasp it as a result of it was written in English, in accordance with Lee. Information shared days later in a small huddle didn’t attain the entire employees, he stated.
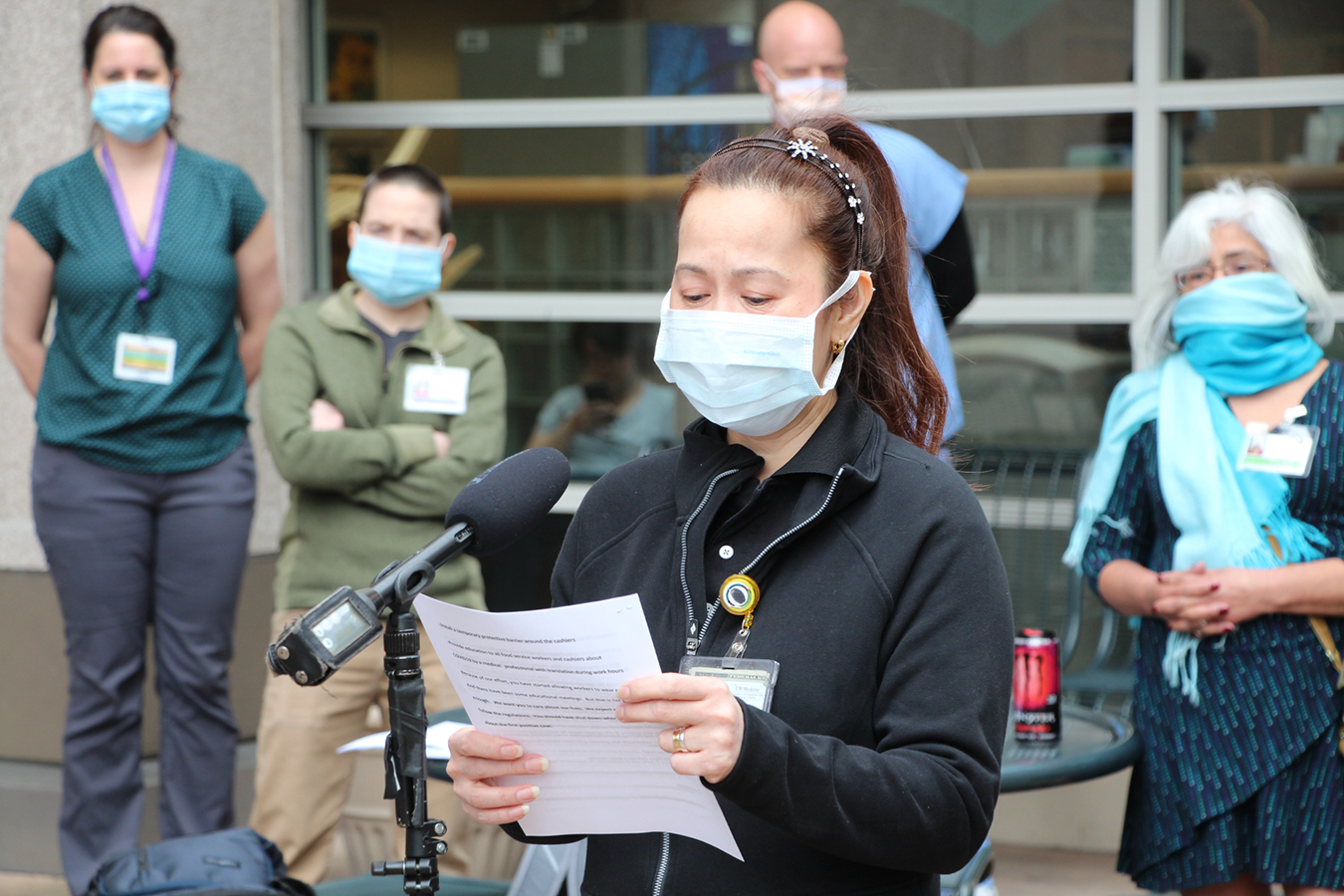
In early April, cafeteria staff delivered a petition to hospital administration, with the assist of WFSE and Service Employees International Union Local 925, with 450 signatures. They requested the hospital shut the Plaza Cafe for a deep cleansing, set up a brief protecting barrier across the cashiers and usher in a medical skilled to teach all cafeteria employees about COVID-19, with translations in different languages.
The cafeteria was not closed, however Mankowski stated the hospital has disinfected it and all workstations, and now requires staff all through the hospital to put on masks. The hospital has declined to put in Plexiglas boundaries on the cafeteria, she stated, as a result of it believes the common masking affords the mandatory security precautions.
The Occupational Safety and Health Administration has no rule requiring that employers inform staff of exposures to infectious ailments. But Dr. Alyssa Burgart, a bioethicist at Stanford, stated hospitals do have an moral obligation. She acknowledged the challenges: With dozens of staff going out and in of a affected person’s room every day, monitoring each single one may be tough, significantly with restricted assets. Hospitals try to determine in actual time precisely what they should disclose and do it.
“Everything is a disaster now, and no one has time to answer anything. So you’re seeing organizations fumble when figuring out how to do this in a way that meets their ethical obligation to protect employees but doesn’t violate federal privacy laws,” Burgart stated.
“The typical way these decisions would be made would be over a very long deliberative process, and that is a luxury we do not have right now. Some organizations are going to miss the mark the first time.”