[partner-box]Younger individuals are much less more likely to be hospitalized or die of COVID-19 than their elders, however they flow into extra freely whereas carrying the illness, and their instances are tougher to hint. Together, these details terrify California hospital officers.
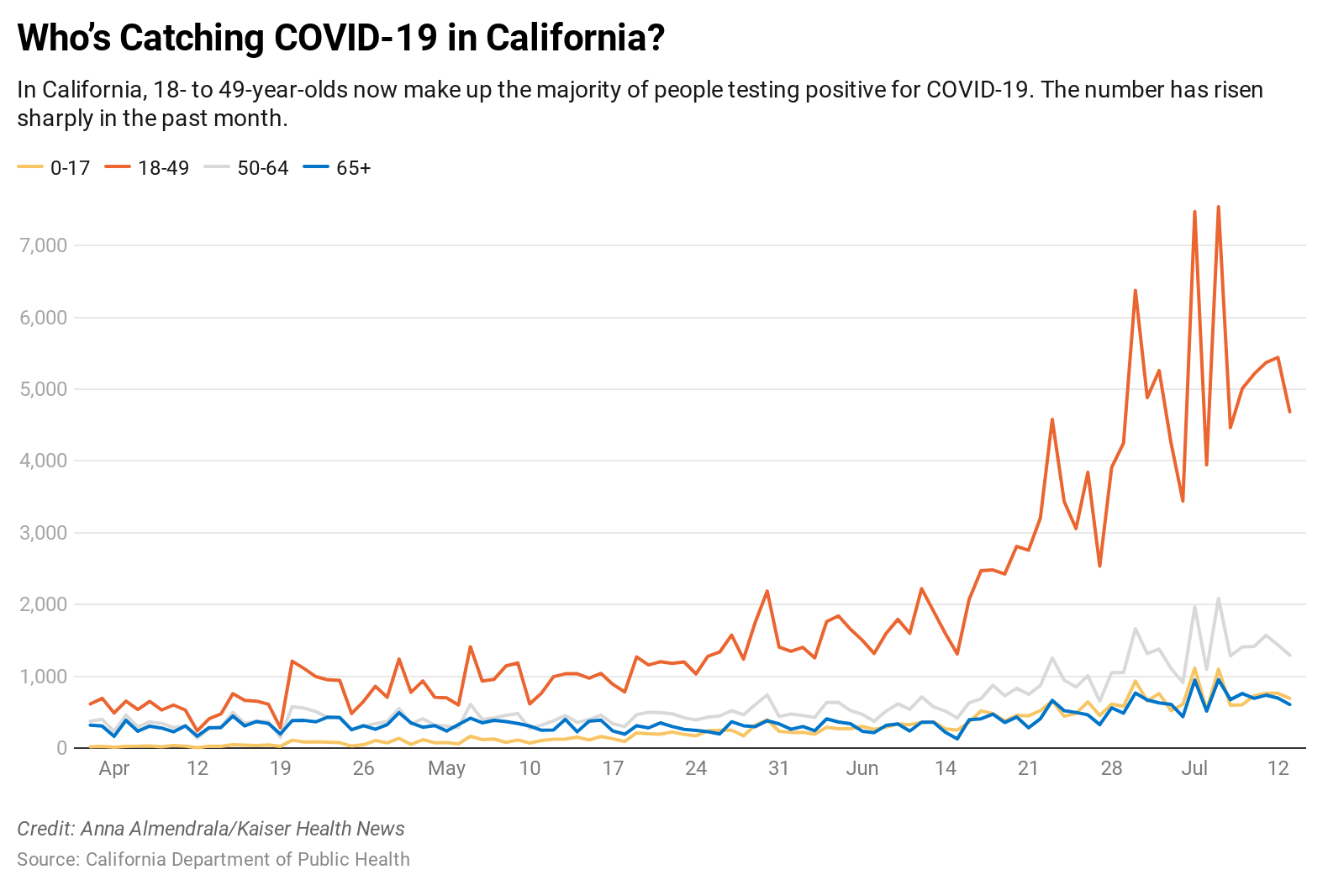
People underneath 50 make up 73% of these testing optimistic for the illness within the state for the reason that starting of June, in contrast with 52% earlier than April 30. That shift isn’t comforting to Dr. Alan Williamson, chief medical officer of Eisenhower Health in Riverside County’s Coachella Valley.
“It honestly worries me more because it means that this is now established in the community,” he stated.
As the virus spreads all through the United States, determining how sufferers had been uncovered turns into more and more troublesome, which makes it almost not possible to cease viral transmission. Younger individuals with COVID-19 are additionally much less more likely to choose up the cellphone when a contact tracer calls, well being officers say. And hospitals are seeing case numbers rise amongst staffers, who’re getting contaminated of their communities, not essentially at work.
Los Angeles and close by counties, whose populations are closely Latino, have been driving California’s COVID spike and account for a disproportionate variety of its instances, as they’ve for the reason that pandemic’s early days.
The huge wave of recent infections has triggered deaths amongst individuals ages 18 to 40 to slowly mount, from six within the first 10 days of May in Los Angeles County, for instance, to 22 in the identical interval of July.
Hospitalizations have soared among the many youthful age group, which made up about 10% of individuals hospitalized in April however account for greater than 25% now. Los Angeles County reported Wednesday that 2,193 individuals had been hospitalized with the virus, the best quantity for the reason that pandemic began. It gave no detailed age breakdown.
The first wave of sufferers in March and April at Eisenhower Medical Center, Eisenhower Health’s 463-bed flagship hospital, had been principally nursing house residents and retirees who lived within the space half time. Most had been white.
But in June, because the virus unfold by way of the remainder of the Coachella Valley — well-known for producing dates, citrus and different crops — it additionally sickened individuals from the area’s year-round Latino agricultural workforce. While these sufferers are youthful and normally don’t want hospitalization, Williamson has seen a brand new development amongst those that do.
“Quite frequently, there would be in their history that there are two or three or more other family members that are home and COVID-positive,” he stated. “I didn’t see that before.”
[khn_slabs slabs=”790331″ view=”inline” /]
In the japanese a part of the valley, the place multigenerational or multifamily households are widespread, COVID-positive sufferers don’t at all times have the house or sources to dwell in strict isolation as they recuperate.
“These are young people living in a household with little kids, teenagers and 70-year-old grandparents,” he stated. “That’s not a good formula.”
Most of the youthful sufferers have a benign course of sickness. Johnny Luna, 34, who lives in a two-bedroom house within the Boyle Heights part close to downtown Los Angeles, acquired examined for COVID-19 in May after experiencing what felt like a gentle bronchial asthma assault, with shortness of breath and fatigue.
When he acquired a letter with a optimistic check consequence every week later, Luna was dumbfounded. He had no concept the place he might need been uncovered, since he, his companion and school-age daughter had adopted public well being suggestions to the letter.
“I washed my hands until they were chapped and dried, and took all the suggested measures,” he stated. “In fact, this was the only thing in my entire life that’s gotten me to stop biting my nails.”
As instances mount, contact tracers are having much less success getting COVID-positive sufferers to choose up the cellphone, stated Dr. Jeffrey Gunzenhauser, chief medical officer on the Los Angeles County Department of Public Health. Contact tracers had been capable of full an interview with optimistic sufferers greater than 70% of the time up till about three weeks in the past, he stated. Now, the speed is as little as 65%.
“It could be that older individuals who traditionally use phones are more willing to answer phones, whereas younger people might communicate through texting and other means, so maybe they’re less likely to,” he stated.
To improve pickups, the division has requested phone corporations to label all calls from contact tracers as “LA Public Health” once they flash on a cellphone’s show. The division has convened focus teams amongst younger adults to determine methods to raised talk with them.
In Luna’s case, AltaMed Health Services, which administered his COVID-19 check, stated it tried to name him three days in a row and left two voicemails earlier than sending the letter. Luna stated that he by no means acquired the calls or voicemails — and that the identical factor occurred to individuals he is aware of.
At the start of the pandemic, contaminated sufferers normally had sense of the place they had been uncovered to the virus, and by whom, stated Patricia Marquez Sung, an epidemiologist with USC Verdugo Hills Hospital, a 158-bed facility in Glendale, in L.A. County.
People exhibiting up on the Verdugo Hills emergency division with COVID signs in June had been considerably youthful than earlier this yr, hospital information reveals — and extra ER sufferers say they’ve “no idea” the place they may have contracted the virus, Sung stated.
“What that’s telling me is that, potentially, we’re getting a little bit lax with the vigilance in masking, staying home and hand-washing,” Sung stated. “People have
gotten stressed and their perceptions of danger are loads decrease than three or 4 months in the past.”
Even well being care staff are getting stressed and venturing out extra. Verdugo Hills’ sister hospital, the 401-bed Keck Hospital of USC close to downtown L.A., is seeing an increase in well being care employee infections from group unfold. During the final 10 days of June, 20 staffers examined optimistic; the hospital’s in-house contact tracing staff decided that none of them had been uncovered to COVID-19 sufferers at work. In the earlier 3½ months the hospital had recorded a complete of 68 positives amongst employees.
Public well being officers and political leaders are urging youthful individuals to chorus from events and huge gatherings, and emphasizing the potential of asymptomatic or pre-symptomatic transmission to extra weak populations.
These cautionary messages are particularly pressing amid a rising consensus that the virus can linger within the air indoors, stated Chris Van Gorder, CEO of Scripps Health, a big nonprofit well being system in San Diego County. Previously, main public well being teams just like the World Health Organization had stated the virus was principally transmitted straight from individual to individual, in respiratory droplets that quickly sink to the bottom until they’re inhaled.
The shift in considering has painful implications for individuals — together with well being care staff — wanting to return to indoor restaurant eating and different companies, stated Van Gorder. Some 201 COVID-19 infections had been reported amongst county well being care staff within the first week of July, in contrast with 72 within the final week of May.
Van Gorder realized that some hospital workers went to casinos once they reopened, and one other group “decided to go off to dinner together in Little Italy. They know better, and they got sick.”
“I think California was doing a phenomenal job flattening the curve, but there was so much pressure to reopen that we reopened too fast,” he stated. “We’re seeing the consequences of that now.”
This story might be republished without cost (details). Younger individuals are much less more likely to be hospitalized or die of COVID-19 than their elders, however they flow into extra freely whereas carrying the illness, and their instances are tougher to hint. Together, these details terrify California hospital officers.
People underneath 50 make up 73% of these testing optimistic for the illness within the state for the reason that starting of June, in contrast with 52% earlier than April 30. That shift isn’t comforting to Dr. Alan Williamson, chief medical officer of Eisenhower Health in Riverside County’s Coachella Valley.
“It honestly worries me more because it means that this is now established in the community,” he stated.
As the virus spreads all through the United States, determining how sufferers had been uncovered turns into more and more troublesome, which makes it almost not possible to cease viral transmission. Younger individuals with COVID-19 are additionally much less more likely to choose up the cellphone when a contact tracer calls, well being officers say. And hospitals are seeing case numbers rise amongst staffers, who’re getting contaminated of their communities, not essentially at work.
Los Angeles and close by counties, whose populations are closely Latino, have been driving California’s COVID spike and account for a disproportionate variety of its instances, as they’ve for the reason that pandemic’s early days.
The huge wave of recent infections has triggered deaths amongst individuals ages 18 to 40 to slowly mount, from six within the first 10 days of May in Los Angeles County, for instance, to 22 in the identical interval of July.
Hospitalizations have soared among the many youthful age group, which made up about 10% of individuals hospitalized in April however account for greater than 25% now. Los Angeles County reported Wednesday that 2,193 individuals had been hospitalized with the virus, the best quantity for the reason that pandemic began. It gave no detailed age breakdown.
The first wave of sufferers in March and April at Eisenhower Medical Center, Eisenhower Health’s 463-bed flagship hospital, had been principally nursing house residents and retirees who lived within the space half time. Most had been white.
But in June, because the virus unfold by way of the remainder of the Coachella Valley — well-known for producing dates, citrus and different crops — it additionally sickened individuals from the area’s year-round Latino agricultural workforce. While these sufferers are youthful and normally don’t want hospitalization, Williamson has seen a brand new development amongst those that do.
“Quite frequently, there would be in their history that there are two or three or more other family members that are home and COVID-positive,” he stated. “I didn’t see that before.”
In the japanese a part of the valley, the place multigenerational or multifamily households are widespread, COVID-positive sufferers don’t at all times have the house or sources to dwell in strict isolation as they recuperate.
“These are young people living in a household with little kids, teenagers and 70-year-old grandparents,” he stated. “That’s not a good formula.”
Most of the youthful sufferers have a benign course of sickness. Johnny Luna, 34, who lives in a two-bedroom house within the Boyle Heights part close to downtown Los Angeles, acquired examined for COVID-19 in May after experiencing what felt like a gentle bronchial asthma assault, with shortness of breath and fatigue.
When he acquired a letter with a optimistic check consequence every week later, Luna was dumbfounded. He had no concept the place he might need been uncovered, since he, his companion and school-age daughter had adopted public well being suggestions to the letter.
“I washed my hands until they were chapped and dried, and took all the suggested measures,” he stated. “In fact, this was the only thing in my entire life that’s gotten me to stop biting my nails.”
As instances mount, contact tracers are having much less success getting COVID-positive sufferers to choose up the cellphone, stated Dr. Jeffrey Gunzenhauser, chief medical officer on the Los Angeles County Department of Public Health. Contact tracers had been capable of full an interview with optimistic sufferers greater than 70% of the time up till about three weeks in the past, he stated. Now, the speed is as little as 65%.
“It could be that older individuals who traditionally use phones are more willing to answer phones, whereas younger people might communicate through texting and other means, so maybe they’re less likely to,” he stated.
To improve pickups, the division has requested phone corporations to label all calls from contact tracers as “LA Public Health” once they flash on a cellphone’s show. The division has convened focus teams amongst younger adults to determine methods to raised talk with them.
In Luna’s case, AltaMed Health Services, which administered his COVID-19 check, stated it tried to name him three days in a row and left two voicemails earlier than sending the letter. Luna stated that he by no means acquired the calls or voicemails — and that the identical factor occurred to individuals he is aware of.
At the start of the pandemic, contaminated sufferers normally had sense of the place they had been uncovered to the virus, and by whom, stated Patricia Marquez Sung, an epidemiologist with USC Verdugo Hills Hospital, a 158-bed facility in Glendale, in L.A. County.
People exhibiting up on the Verdugo Hills emergency division with COVID signs in June had been considerably youthful than earlier this yr, hospital information reveals — and extra ER sufferers say they’ve “no idea” the place they may have contracted the virus, Sung stated.
“What that’s telling me is that, potentially, we’re getting a little bit lax with the vigilance in masking, staying home and hand-washing,” Sung stated. “People have
gotten stressed and their perceptions of danger are loads decrease than three or 4 months in the past.”
Even well being care staff are getting stressed and venturing out extra. Verdugo Hills’ sister hospital, the 401-bed Keck Hospital of USC close to downtown L.A., is seeing an increase in well being care employee infections from group unfold. During the final 10 days of June, 20 staffers examined optimistic; the hospital’s in-house contact tracing staff decided that none of them had been uncovered to COVID-19 sufferers at work. In the earlier 3½ months the hospital had recorded a complete of 68 positives amongst employees.
Public well being officers and political leaders are urging youthful individuals to chorus from events and huge gatherings, and emphasizing the potential of asymptomatic or pre-symptomatic transmission to extra weak populations.
These cautionary messages are particularly pressing amid a rising consensus that the virus can linger within the air indoors, stated Chris Van Gorder, CEO of Scripps Health, a big nonprofit well being system in San Diego County. Previously, main public well being teams just like the World Health Organization had stated the virus was principally transmitted straight from individual to individual, in respiratory droplets that quickly sink to the bottom until they’re inhaled.
The shift in considering has painful implications for individuals — together with well being care staff — wanting to return to indoor restaurant eating and different companies, stated Van Gorder. Some 201 COVID-19 infections had been reported amongst county well being care staff within the first week of July, in contrast with 72 within the final week of May.
Van Gorder realized that some hospital workers went to casinos once they reopened, and one other group “decided to go off to dinner together in Little Italy. They know better, and they got sick.”
“I think California was doing a phenomenal job flattening the curve, but there was so much pressure to reopen that we reopened too fast,” he stated. “We’re seeing the consequences of that now.”