Months into a brand new Biden administration coverage meant to decrease drug prices for Medicare sufferers, impartial pharmacists say they’re struggling to afford to maintain some pharmaceuticals in inventory.
“It would not matter if the governor himself walked in and said, ‘I need to get this prescription filled,’” mentioned Clint Hopkins, a pharmacist and co-owner of Pucci’s Pharmacy in Sacramento, California. “If I’m losing money on it, it’s a no.”
A regulation that took impact in January adjustments prescription costs for Medicare beneficiaries. For years, costs included pharmacy efficiency incentives, attainable rebates, and different changes made after the prescription was crammed. Now the changes are made first, on the pharmacy counter, decreasing the general price for sufferers and the federal government. But the brand new system means much less cash for pharmacies that purchase and inventory medicines, pharmacists say.
Pharmacies are already combating employees shortages, drug shortages, fallout from opioid lawsuits, and rising working prices. While impartial pharmacies are most susceptible, some huge chain pharmacies are additionally feeling a money crunch — significantly these whose dad or mum corporations don’t personal a pharmacy profit supervisor, corporations that negotiate drug costs between insurers, drug producers, and pharmacies.
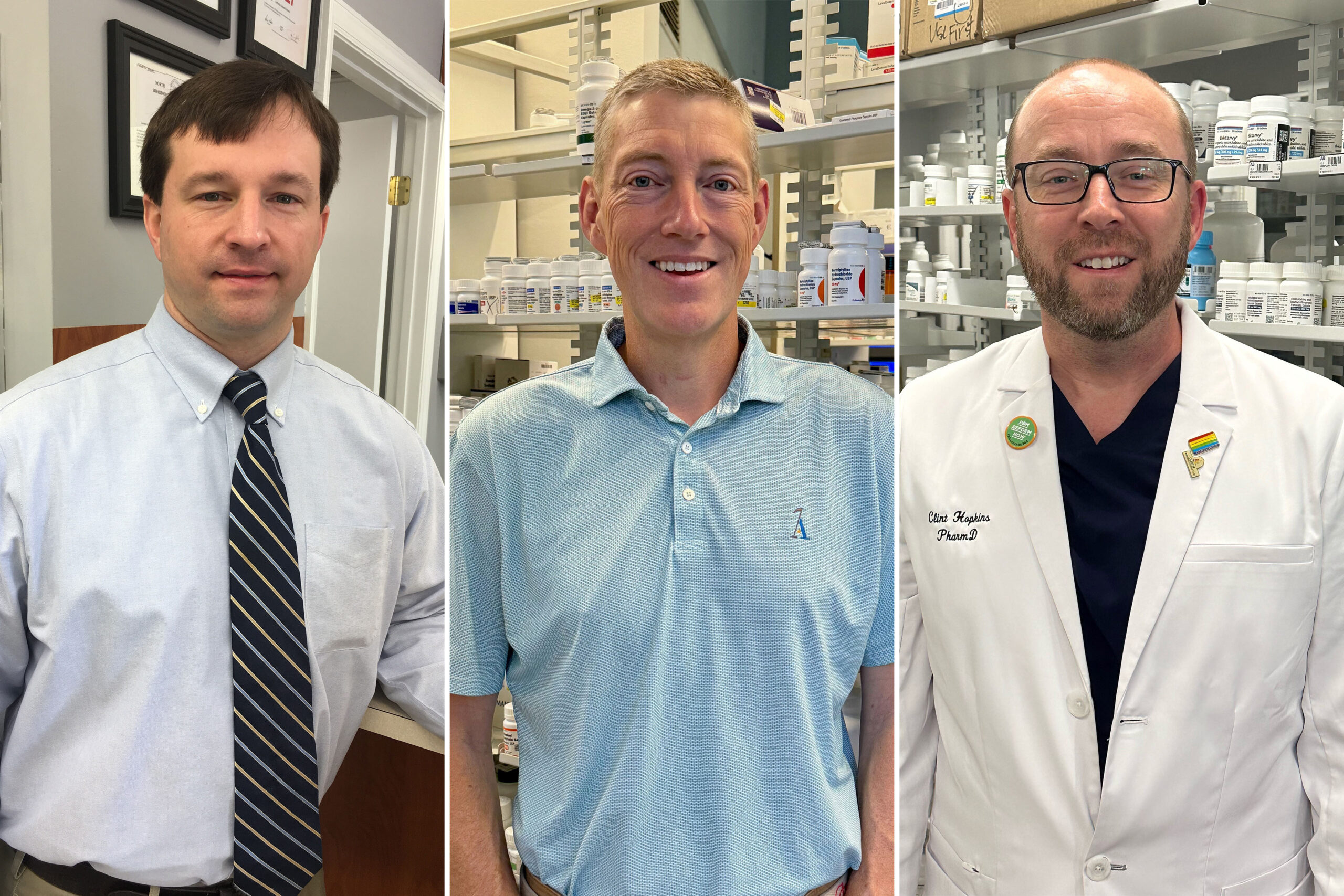
“It would not matter if the governor himself walked in and said, ‘I need to get this prescription filled,’” says Clint Hopkins, a Sacramento, California, pharmacist. “If I’m losing money on it, it’s a no.”(Joel Hockman)
A prime official on the Centers for Medicare & Medicaid Services mentioned it’s a matter for pharmacies, Medicare insurance coverage, and PBMs to resolve.
“We cannot interfere in the negotiations that occur between the plans and pharmacy benefits managers,” Meena Seshamani, director of the Center for Medicare, mentioned at a convention on June 7. “We cannot tell a plan how much to pay a pharmacy or a PBM.”
Nevertheless, CMS has reminded insurers and PBMs in a number of letters that they’re required to supply the medicine and different advantages promised to beneficiaries.
Several impartial pharmacists advised KFF Health News they’ll quickly reduce on the variety of medicines they carry on cabinets, significantly brand-name medicine. Some have even determined to cease accepting sure Medicare drug plans, they mentioned.
As he campaigns for reelection, President Joe Biden has touted his administration’s strikes to make pharmaceuticals extra reasonably priced for Medicare sufferers, hoping to attraction to voters troubled by rising well being care prices. His achievements include a law, the Inflation Reduction Act, that caps the worth of insulin at $35 a month for Medicare sufferers; caps Medicare sufferers’ drug spending at $2,000 a yr, starting subsequent yr; and permits this system to cut price down drug costs with producers.
More than 51 million individuals have Medicare drug protection. CMS officers estimated the brand new rule decreasing pharmacy prices would save beneficiaries $26.5 billion from 2024 via 2032.
Medicare sufferers’ prescriptions can account for a minimum of 40% of pharmacy enterprise, in line with a February survey by the National Community Pharmacists Association.
Independent pharmacists say the brand new rule is inflicting them monetary bother and hardship for some Medicare sufferers. Hopkins, in Sacramento, mentioned that a few of his newer clients used to depend on a neighborhood grocery pharmacy however got here to his retailer after they may now not get their medicines there.
The crux of the issue is money circulation, the pharmacists say. Under the previous system, pharmacies and PBMs reconciled rebates and different behind-the-scenes transactions a couple of occasions a yr, leading to pharmacies refunding any overpayments.
Now, PBM clawbacks occur instantly, with each crammed prescription, decreasing pharmacies’ money readily available. That has made it significantly troublesome, pharmacists say, to inventory brand-name medicine that may price tons of or hundreds of {dollars} for a month’s provide.
Some sufferers have been compelled to decide on between their pharmacy and their drug plan. Kavanaugh Pharmacy in Little Rock, Arkansas, now not accepts Cigna and Wellcare Medicare drug plans, mentioned co-owner and pharmacist Scott Pace. He mentioned the pharmacy made the change as a result of the businesses use Express Scripts, a PBM that has lower its reimbursements to pharmacies.
“We had a lot of Wellcare patients in 2023 that either had to switch plans to remain with us, or they had to find a new provider,” Pace mentioned.
Pharmacist Scott Pace, of Little Rock, Arkansas, now not accepts two Medicare drug plans due to low reimbursements.(Kori Gordon)
Pace mentioned one affected person’s drug plan not too long ago reimbursed him for a fentanyl patch $40 lower than his price to amass the drug. “Because we’ve had a long-standing relationship with this particular patient, and they’re dying, we took a $40 loss to take care of the patient,” he mentioned.
Conceding that some pharmacies face cash-flow issues, Express Scripts not too long ago determined to speed up cost of bonuses for assembly the corporate’s efficiency measures, mentioned spokesperson Justine Sessions. She declined to reply questions on cuts in pharmacy funds.
Express Scripts, which is owned by The Cigna Group, managed 23% of prescription claims final yr, second to CVS Health, which had 34% of the market.
In North Carolina, pharmacist Brent Talley mentioned he not too long ago misplaced $31 filling a prescription for a month’s provide of a weight management and diabetes drug.
To attempt to cushion such losses, Talley’s Hayes Barton Pharmacy sells CBD merchandise and specialty gadgets like studying glasses, bathtub merchandise, and books about native historical past. “But that’s not going to come close to making up the loss generated by the prescription sale,” Talley mentioned.
His pharmacy additionally delivers medicines packaged by the dose to Medicare sufferers at assisted dwelling services and nursing properties. Reimbursement preparations with PBMs for that enterprise are extra favorable than for filling prescriptions in individual, he mentioned.
Brent Talley, a Raleigh, North Carolina, pharmacist, says that, whereas his retailer sells quite a lot of specialty gadgets, “that’s not going to come close to making up the loss generated by the prescription sale.”(Elizabeth Talley)
When Congress added drug protection to Medicare in 2003, lawmakers privatized the profit by requiring the federal government to contract with business insurance coverage corporations to handle this system.
Insurers supply two choices: Medicare Advantage plans, which often cowl medicines, along with hospital care, physician visits, and different providers; in addition to stand-alone drug plans for individuals with conventional Medicare. The insurers then contract with PBMs to barter drug costs and pharmacy prices with drug producers and pharmacies.
The phrases of PBM contracts are typically secret and limit what pharmacists can inform sufferers — for instance, in the event that they’re requested why a drug is out of inventory. (It took an act of Congress in 2018 to eradicate restrictions on disclosing a drug’s money value, which may generally be lower than an insurance coverage plan’s copayment.)
The Pharmaceutical Care Management Association, a commerce group representing PBMs, warned CMS repeatedly “that pharmacies would likely receive lower payments under the new Medicare Part D rule,” spokesperson Greg Lopes mentioned. His group opposes the change.
Recognizing the brand new coverage might trigger cash-flow issues for pharmacies, Medicare officers had delayed implementation for a yr earlier than the rule took impact, giving them extra time to regulate.
“We have heard pharmacies saying that they have concerns with their reimbursement,” Seshamani mentioned.
But the company isn’t doing sufficient to assist now, mentioned Ronna Hauser, senior vice chairman of coverage and pharmacy affairs on the National Community Pharmacists Association. “They haven’t taken any action even after we brought potential violations to their attention,” she mentioned.
Susan Jaffe:
[email protected],
@susanjaffe
Related Topics
src=”//platform.twitter.com/widgets.js” charset=”utf-8″>