Jordan Rau, KFF Health News
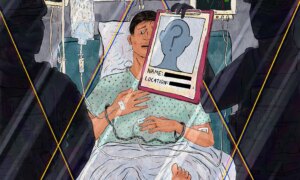
On trip in Mexico final yr, Michael DiPlacido handed out twice whereas scuba diving and once more in his resort. Back in St. Louis, docs identified him with amyotrophic lateral sclerosis, or ALS, an incurable illness that always requires mechanical air flow.
When his son Adam DiPlacido tried to discover a everlasting place to look after his father, who now wanted a ventilator to breathe by a tracheostomy tube, he found none of Missouri’s almost 500 nursing houses might take him.
“I never thought it would be easy, but I never thought it would be this hard,” Adam mentioned.
A KFF Health News investigation discovered widespread flaws and gaps in look after a few of the nation’s most debilitated folks: those that can not breathe on their very own.
Spinal wire accidents, strokes, continual obstructive pulmonary illness, and neurological illnesses similar to a number of sclerosis have left tens of 1000’s of Americans completely depending on ventilators. The limitations these sufferers face supply a stark instance of how the United States’ disjointed well being care system makes coping with extreme sickness a lot more durable.
The investigation discovered sufferers are continuously stymied in efforts to get their insurers to offer applicable dwelling ventilators. They can find yourself spending a whole bunch of 1000’s of {dollars} for personal nurses to verify they don’t die in a single day. Those who must be in a nursing dwelling or different well being facility generally should transfer to a different state, removed from their households.
“There are not a lot of institutions that can manage these people,” mentioned Jonathon Schwartz, appearing chief medical officer for the Spaulding Rehabilitation Network in Boston.
Only 347 of the nation’s roughly 14,750 nursing houses have specialised items devoted to folks on ventilators, a KFF Health News evaluation of federal knowledge exhibits. Fifteen states, together with Missouri, don’t have any nursing houses with a specialised unit for ventilator care.
While nursing houses can look after residents on ventilators on their common flooring, in observe few do. From April by June, fewer than 10% of nursing houses had long-stay residents respiratory with the help of invasive mechanical ventilators, which ship air by a tube down the airway or through a tracheostomy, the evaluation discovered. Fewer than 15% of nursing houses had short-stay sufferers on ventilators.
Many sufferers in nursing houses could be weaned off ventilators, however those that can’t due to their situation usually spend years in hospitals, which aren’t designed for residency. Innovative alternate options to conventional nursing houses exist in some areas of the nation, however they haven’t been broadly replicated and now are in danger from steep reductions in Medicaid enacted by President Donald Trump and the Republican-controlled Congress.
“It could create a terrible scenario,” mentioned Gene Gantt, a respiratory care advisor to states and insurers.
Many folks completely on ventilators favor to reside at dwelling so long as they will. But care there could be perilous and dear. Some state well being applications pay for ventilator look after low-income sufferers, however getting enrolled can take months amid bureaucratic hurdles and waitlists.
Some insurers balk at offering superior dwelling ventilators — which sound alerts for collapsed lungs, airway leaks, or malfunctions and may price greater than $10,000 — till sufferers have misplaced a lot of their skill to breathe.
“Feeling you’re suffocating is a horrific feeling, and that feeling can go on for months and months” as ALS sufferers decline whereas sparring with insurers, mentioned Tyler Rehbein, an assistant professor of neurology on the University of Rochester who treats ALS sufferers.
‘Out of Money’
David Goldstein’s first symptom of ALS was a limp that appeared within the fall of 2022. It took six months for docs to diagnose him with the neuromuscular dysfunction, also referred to as Lou Gehrig’s Disease. ALS afflicts about 34,000 Americans, destroying the nerve cells within the mind and spinal wire that management muscle tissue, together with these for respiratory. It finally ends in full paralysis, whereas most individuals stay mentally alert. Patients normally find yourself on ventilators if they don’t die first, and respiratory failure is the most typical reason behind dying.
Now 69 and on a ventilator, David can not transfer something besides his eyes and mouth, mentioned his ex-wife, Janis Goldstein, who has energy of lawyer. He requires somebody round on a regular basis in his Houston condo to feed and bathe him, give him medicine, and take away mucus blocking his airway. The settings on the ventilator require frequent monitoring and changes.
In spring of 2023, David acquired on the ready record for Texas’ Medicaid dwelling well being program for disabled adults. More than a yr later, Texas licensed 12 hours of dwelling care a day. Still, Janis mentioned, the state’s designated administrator generally has hassle getting employees for these shifts, and she or he and her ex-husband should pay for nurses to cowl the remainder of the day or evening.
She mentioned they’ve spent round a half-million {dollars}, largely on nurses and aides. They raised a lot of it by on-line campaigns and a fundraiser headlined by the nation singer Larry Gatlin.
“The point that we’re at now, with the 24-hour help, is we’re pretty much out of money,” Janis mentioned.
She is planning to maneuver David into one of many few nursing houses within the area that take sufferers on ventilators, she mentioned, however is worried will probably be tough to rearrange for somebody to stick with David in a single day in his room. She fears that if David’s place shifts even half an inch, he received’t have the ability to name for assist by the machine that tracks his eye actions.
“I don’t know that he’ll be able to handle the stress and the anxiety of knowing that he could suffocate, even in a facility, because he doesn’t have someone by his side,” she mentioned.
Ventilator Deserts
When Michael DiPlacido’s son Adam spent weeks trying to find a facility in Missouri that would handle a affected person on a ventilator with a trach tube, the one one which was even a risk instructed him it couldn’t settle for new sufferers, as a result of its lone respiratory therapist had give up.
“It’s incredible to me there is not one single place in Missouri that can take a patient like my father,” Adam mentioned.
Looking exterior the state, Michael determined to maneuver to a nursing dwelling north of Chicago, about 5 hours by automotive from St. Louis. After three months, he left the power as a result of it was so far-off from his household, Adam mentioned.
Adam helped his father transfer right into a long-term care hospital in suburban St. Louis for six weeks. But Michael’s insurer wouldn’t pay for hospital-level acute care, so Adam mentioned Michael needed to pay greater than $47,000 out-of-pocket. Next, Adam helped him transfer to a different Illinois nursing dwelling, about an hour away, that his son had initially rejected due to on-line critiques, together with a Medicare warning that abuse had occurred. Finding it poor, Michael left after every week.
Adam discovered a personal nursing dwelling firm that might look after Michael in his dwelling, at a price of $960 a day. “After 323 days, my father has finally made it back home,” Adam mentioned in an e mail in September.
But along with his well being quickly deteriorating, Michael was admitted to a hospice facility in October. He died later that month at 75.
Gantt, the respiratory care advisor, mentioned that fewer than half of state Medicaid applications present satisfactory reimbursement charges for ventilator sufferers. He mentioned most state Medicaid cost formulation don’t measure outcomes or reward nursing houses financially if they supply higher care, similar to weaning a affected person off the ventilator or stopping infections. He mentioned he has seen nursing houses settle for sufferers with trach tubes even when nurses lack correct coaching, or when the power doesn’t make use of respiratory therapists.
“For the large part, these patients are stuck in bed,” Gantt mentioned. “We should try to get them the best quality of life.”
David Gifford, the chief medical officer for the American Health Care Association, a nursing dwelling commerce group, mentioned equipping a nursing dwelling with ventilators and getting state approval is dear, and outdoors of city areas, many markets lack sufficient native sufferers who want ventilators to make it financially worthwhile.
“It’s not as simple as saying we’re going to pay more and have more respiratory therapists,” Gifford mentioned. “This is a group that needs highly specialized care. You’re not going to have it everywhere.”
Flagging Breaths
Derek McManus’ weakening proper hand and occasional twitching was the primary signal one thing was incorrect. In October 2023, docs identified Derek, a company government who lives in Painted Post, New York, with ALS.
By August 2024, Derek’s lungs had been working at 78% of capability, his medical information present. Because ALS progresses so rapidly, docs usually prescribe superior home mechanical ventilators. These machines ship high-pressure air by a masks (known as non-invasive) or a tube down the airway or through a tracheostomy (known as invasive). They can calibrate themselves primarily based on a affected person’s respiratory and have alarms that detect leaks, airway blockages, and machine malfunctions. They can run on transportable energy sources and backup batteries in case of an influence failure. The machines can enable folks to speak or eat.
But some insurers have what physicians name “fail first” insurance policies that received’t pay for ventilators except the affected person has already tried a respiratory help machine with out success (as outlined by the corporate). These less complicated machines, the sort sleep apnea sufferers use, are usually not as efficient in eradicating carbon dioxide as ventilators and lack security options. Commonly recognized by the acronyms BiPAP or CPAP, they will price $1,000 or extra and must be plugged into {an electrical} socket.
“It seems to be an expectation of insurance companies they should live the rest of their life attached to a wall outlet,” mentioned Rehbein, the University of Rochester neurologist.
In November 2024, Derek’s insurer denied his doctor’s request for a ventilator, writing that “you have not failed treatment” with the less complicated machine, in keeping with the insurer’s letter, offered by his spouse, Lesley McManus. By April, Derek’s respiratory capability had dropped to 60% of regular. Lesley mentioned she apprehensive he would suffocate in a single day if his primary machine stopped working, because it had no security alert. “He couldn’t take the mask off, because he can’t move his hands,” she mentioned.
The insurer denied a second request for a ventilator, reiterating that Derek had not proven the less complicated machine hadn’t labored, in keeping with one other insurance coverage letter. Derek, who’s 56, appealed to an unbiased medical reviewer, who overturned the insurer’s resolution and ordered it to offer a ventilator, in keeping with a replica of the ruling. The physician wrote that the machine’s alarm system and capability to routinely clear away airway secretion by simulating a cough had been “vital for patient safety” and would assist defend Derek from creating pneumonia.
“This multi-faceted approach to respiratory care is essential for improving gas exchange, reducing the work of breathing, and ultimately enhancing the patient’s quality of life and extending survival,” the choice mentioned.
Derek mentioned that since he acquired the brand new machine, he’s respiratory simpler, actually and emotionally. “If I’m not breathing right, it will give it an alert, and it will let us know if I don’t have the mask on properly,” he mentioned.
The McManus household requested KFF Health News not publish their insurer’s title, out of concern of repercussions.
Insurance Rules
John Hansen-Flaschen, a pulmonologist who based Penn Medicine’s program for home assisted ventilation, mentioned some sufferers hand over when an insurer denies their requests and don’t file appeals. “These are some of the most vulnerable people there are, and they don’t have energy to do this,” he mentioned.
Doctors who deal with sufferers with neuromuscular problems mentioned probably the most resistance to offering ventilators comes from some non-public Medicare Advantage plans, however they mentioned it additionally has been a difficulty with some business insurance policies.
Insurers dispute that they refuse ventilators for sufferers who want them. The written policy of Excellus BlueCross BlueShield, which Rehbein mentioned was one of many firms that covers his sufferers, requires less complicated respiratory machines to have failed earlier than sufferers can get the extra refined ventilator. After a KFF Health News inquiry, Excellus clarified its coverage with a footnote saying it does take into account mechanical ventilators as first-line remedy for sure conditions, similar to ALS, on a case-by-case foundation.
UnitedHealthcare confirmed that a few of its insurance policies require {that a} much less complicated machine be tried initially and located ineffective earlier than a ventilator could be licensed. Aetna’s policy doesn’t mandate a stepped course of and says it considers mechanical ventilators primarily based on the severity of the situation and “where interruption or failure of respiratory support would lead to death,” with different sufferers eligible just for the less complicated units. Humana and Cigna didn’t reply to requests to offer their insurance policies.
Chris Bond, a spokesperson for AHIP, the medical insurance trade’s commerce group, mentioned, “Health plans work to connect patients with safe, clinically appropriate care and welcome opportunities to work with policymakers and stakeholders across the health care system to continually improve access and precisely address any coverage-related issues.”
Melanie Lendnal, senior vp for coverage and advocacy on the ALS Association, mentioned, “I haven’t met one person yet living with ALS, or a family member, who has not had to fight — really fight — to get a non-invasive ventilator.”
A Model in Massachusetts
In 2019, David Marion, a 36-year-old plumber, was hanging out with mates in Lowell, Massachusetts, when he tripped on the sidewalk and fractured his neck. The harm rendered him quadriplegic and paralyzed his stomach and diaphragm muscle tissue, requiring him to make use of a ventilator. Surgeons carried out a tracheotomy, and over the following yr and a half, Marion lived in two long-term acute care hospitals. “I didn’t get out of bed” on the second hospital, Marion, now 43, mentioned in an interview.
His mom, Denise Valliere, who lives in New Hampshire, mentioned she grew determined looking for a everlasting dwelling for him that was shut sufficient that she might go to. “Some of those nursing homes are pretty sad places,” she mentioned.
At the tip of 2020, Marion’s luck turned. He was accepted by the Leonard Florence Center for Living in Chelsea, Massachusetts, which has created a substitute for the institutional life most nursing houses can supply folks on ventilators. The heart follows the Green House philosophy, with small residences every serving 10 folks, with non-public bedrooms, a typical front room, and out of doors house. Residents set their very own schedules, together with when and what to eat. The heart has 10 residences in its constructing; six are devoted to folks depending on ventilators, together with these with ALS or MS.
The heart’s respiratory therapists helped Marion get to the purpose the place he didn’t want a feeding tube and didn’t require his ventilator for parts of the day. The heart offered a transportable ventilator hooked up to his wheelchair and a pc pill that Marion operates along with his mouth. It permits him to summon the elevator, open doorways, go exterior, and regulate his mattress, window shades, temperature, and tv settings. Other residents who can’t use their palms or mouths can function the units by a digital camera that captures eye motion.
“This gives back independence to people who never thought they’d have independence again,” mentioned Barry Berman, the chief government officer of Chelsea Jewish Lifecare, the nonprofit that owns the Leonard Florence Center. “There are alternatives. It doesn’t have to be the way that it is.”
Most of the residents’ stays are paid for by Medicaid, which along with Medicare offers the majority of the middle’s income. Its funds are bolstered by the nonprofit’s endowment, one thing most nursing houses lack. Berman mentioned that because the heart opened in 2010, he has hosted dozens of holiday makers taken with replicating its mannequin elsewhere within the nation, however nobody has.
Some states have licensed amenities that aren’t nursing houses to look after folks on ventilators. In California, some folks on ventilators reside in “congregate living health facilities,” that are residential homes that provide 24-hour skilled nursing for the terminally sick, people who find themselves catastrophically or severely disabled, or people who find themselves mentally alert however bodily disabled.
Patients usually should pay privately as a result of Medicaid managed care applications don’t embody these amenities as a profit, mentioned Mariam Voskanyan, who’s president of the state affiliation representing congregate residing amenities and owns one in Los Angeles. California’s Medi-Cal program is permitted to pay these sorts of amenities by its Home and Community-Based Alternatives waiver, however this system is at capability and there may be a waitlist of greater than 5,000 folks.
Researchers count on states will be under pressure to scale back or remove applications like these to make up for almost $900 billion in coming Medicaid reductions, because the federal authorities doesn’t require states to cowl respiratory care for people on ventilators or nursing home alternatives.
Valliere, Marion’s mom, mentioned she was baffled that there have been no more locations like Leonard Florence. “How can we be so behind in that kind of care and those kinds of facilities if we’re the best country in the world,” she requested. “Why is this?”
KFF Health News is a nationwide newsroom that produces in-depth journalism about well being points and is likely one of the core working applications at KFF—an unbiased supply of well being coverage analysis, polling, and journalism. Learn extra about KFF.
USE OUR CONTENT
This story could be republished totally free (details).