For the previous 12 months and a half, Tandra Cooper Harris and her husband, Marcus, who each have diabetes, have struggled to fill their prescriptions for the drugs they should management their blood sugar.
Without Ozempic or the same drug, Cooper Harris suffers blackouts, turns into too drained to observe her grandchildren, and struggles to earn more money braiding hair. Marcus Harris, who works as a Waffle House prepare dinner, wants Trulicity to maintain his legs and toes from swelling and bruising.
The couple’s physician has tried prescribing comparable medication, which mimic a hormone that suppresses urge for food and controls blood sugar by boosting insulin manufacturing. But these, too, are sometimes out of inventory. Other occasions, their insurance coverage via the Affordable Care Act market burdens the couple with a prolonged approval course of or an out-of-pocket price they will’t afford.
“It’s like, I’m having to jump through hoops to live,” mentioned Cooper Harris, 46, a resident of Covington, Georgia, east of Atlanta.
Supply shortages and insurance coverage hurdles for this highly effective class of medication, known as GLP-1 agonists, have left many people who find themselves affected by diabetes and weight problems with out the medicines they should keep wholesome.
One root of the issue is the very excessive costs set by drugmakers. About 54% of adults who had taken a GLP-1 drug, together with these with insurance coverage, mentioned the fee was “difficult” to afford, in line with KFF poll results launched this month. But it’s sufferers with the bottom disposable incomes who’re being hit the toughest. These are individuals with few assets who wrestle to see docs and purchase wholesome meals.
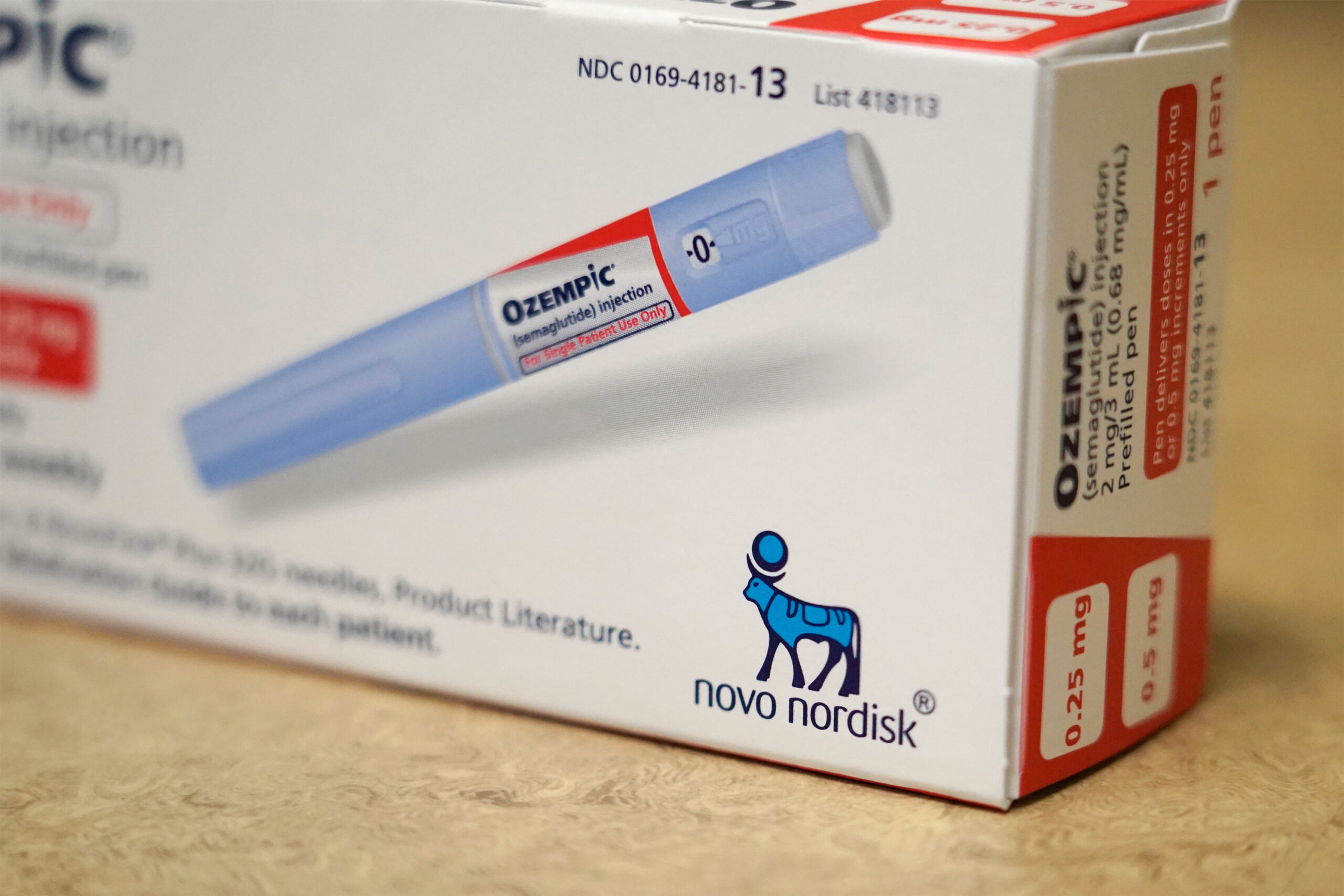
In the United States, Novo Nordisk prices about $1,000 for a month’s provide of Ozempic, and Eli Lilly prices the same quantity for Mounjaro. Prices for a month’s provide of various GLP-1 medication range from $936 to $1,349 earlier than insurance coverage protection, in line with the Peterson-KFF Health System Tracker. Medicare spending for 3 standard diabetes and weight reduction medication — Ozempic, Rybelsus, and Mounjaro — reached $5.7 billion in 2022, up from $57 million in 2018, in line with research by KFF.
The “outrageously high” worth has “the potential to bankrupt Medicare, Medicaid, and our entire health care system,” Sen. Bernie Sanders (I-Vt.), who chairs the U.S. Senate Committee on Health, Education, Labor and Pensions, wrote in a letter to Novo Nordisk in April.
The excessive costs additionally imply that not everybody who wants the medication can get them. “They’re kind of disadvantaged in multiple ways already and this is just one more way,” mentioned Wedad Rahman, an endocrinologist with Piedmont Healthcare in Conyers, Georgia. Many of Rahman’s sufferers, together with Cooper Harris, are underserved, have high-deductible well being plans, or are on public help applications like Medicaid or Medicare.
Many drugmakers have applications that assist sufferers get began and keep on medicines for little or no price. But these applications haven’t been dependable for medicines like Ozempic and Trulicity due to the provision shortages. And many insurers’ necessities that sufferers obtain prior authorization or first attempt cheaper medication add to delays in care.
By the time a lot of Rahman’s sufferers see her, their diabetes has gone unmanaged for years they usually’re affected by extreme problems like foot wounds or blindness. “And that’s the end of the road,” Rahman mentioned. “I have to pick something else that’s more affordable and isn’t as good for them.”
GLP-1 agonists — the class of medication that features Ozempic, Trulicity, and Mounjaro — had been first authorised to deal with diabetes. In the final three years, the Food and Drug Administration has authorised rebranded variations of Mounjaro and Ozempic for weight reduction, main demand to skyrocket. And demand is simply rising as extra of the medication’ advantages develop into obvious.
In March, the FDA authorised the load loss drug Wegovy, a model of Ozempic, to treat heart problems, which can probably improve demand, and spending. Up to 30 million Americans, or 9% of the U.S. inhabitants, are anticipated to be on a GLP-1 agonist by 2030, the monetary companies firm J.P. Morgan estimated.
As extra sufferers attempt to get prescriptions for GLP-1 agonists, drugmakers wrestle to make sufficient doses.
Eli Lilly is urging individuals to keep away from utilizing its drug Mounjaro for beauty weight reduction to make sure sufficient provides for individuals with medical situations. But the medication’ recognition continues to develop regardless of unwanted side effects akin to nausea and constipation, pushed by their effectiveness and movie star endorsements. In March, Oprah Winfrey launched an hourlong particular on the medicines’ capacity to assist with weight reduction.
It can look like everybody on the planet is taking this class of treatment, mentioned Jody Dushay, an assistant professor of medication at Harvard Medical School and an endocrinologist at Beth Israel Deaconess Medical Center. “But it’s kind of not as many people as you think,” she mentioned. “There just isn’t any.”
Even when the medication are in inventory, insurers are clamping down, leaving sufferers and well being care suppliers to navigate a thicket of ever-changing protection guidelines. State Medicaid plans vary in their coverage of the medication for weight reduction. Medicare won’t cover the drugs if they’re prescribed for weight problems. And commercial insurers are tightening access because of the medication’ price.
Health care suppliers are cobbling collectively care plans primarily based on what’s out there and what sufferers can afford. For instance, Cooper Harris’ insurer covers Trulicity however not Ozempic, which she mentioned she prefers as a result of it has fewer unwanted side effects. When her pharmacy was out of Trulicity, she needed to rely extra on insulin as a substitute of switching to Ozempic, Rahman mentioned.
One day in March, Brandi Addison, an endocrinologist in Corpus Christi, Texas, needed to alter the prescriptions for all 18 of the sufferers she noticed due to points with drug availability and price, she mentioned. One affected person, insured via a trainer retirement well being plan with a excessive deductible, couldn’t afford to be on a GLP-1 agonist, Addison mentioned.
“Until she reaches that deductible, that’s just not a medication she can use,” Addison mentioned. Instead, she put her affected person on insulin, whose worth is capped at a fraction of the price of Ozempic, however which doesn’t have the identical advantages.
“Those patients who have a fixed income are going to be our more vulnerable patients,” Addison mentioned.
Renuka Rayasam:
[email protected],
@renurayasam
Related Topics
src=”//platform.twitter.com/widgets.js” charset=”utf-8″>