Judith Graham
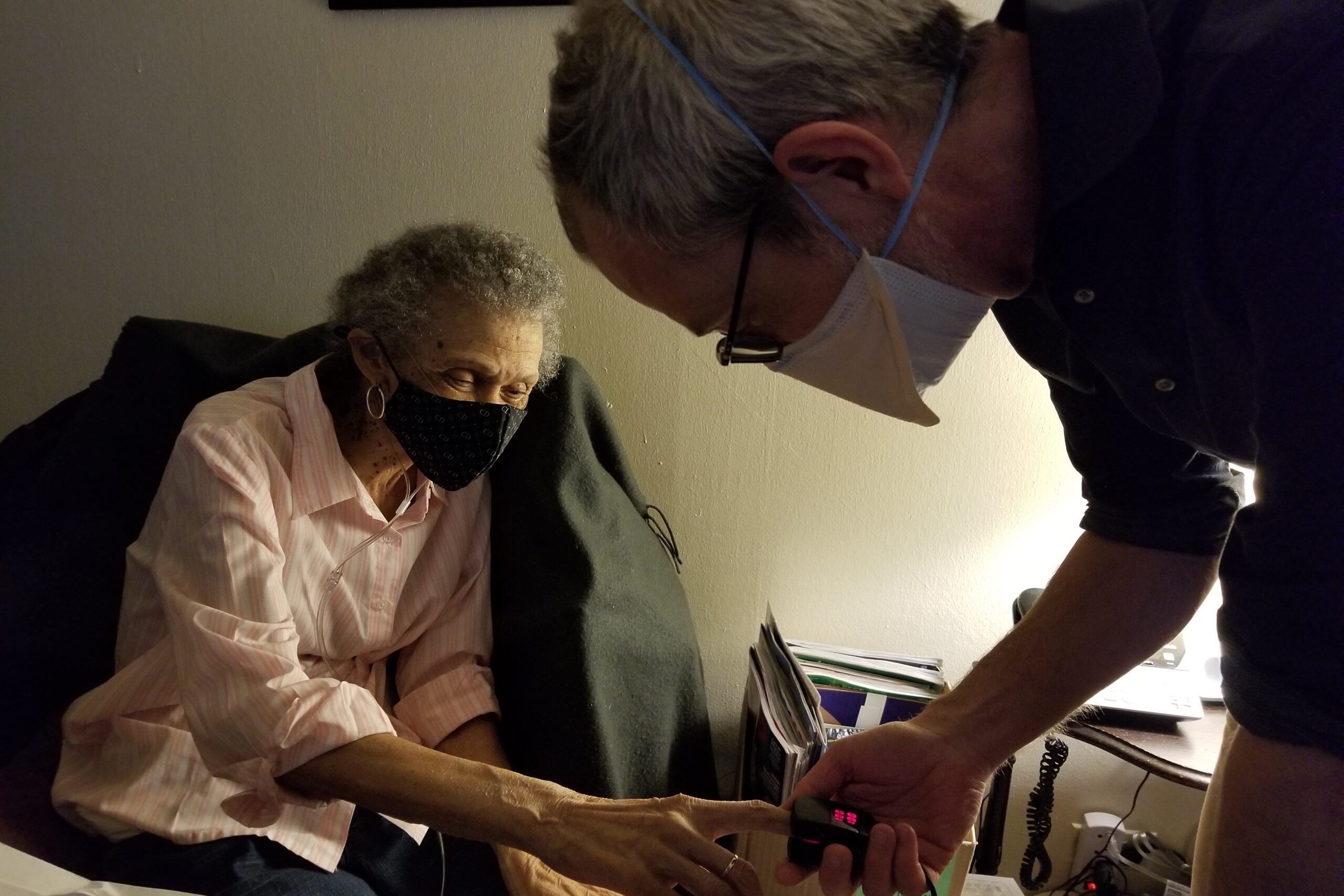
Carolyn Dickens, 76, was sitting at her eating room desk, struggling to catch her breath as her doctor seemed on with concern.
“What’s going on with your breathing?” requested Peter Gliatto, director of Mount Sinai’s Visiting Doctors Program.
“I don’t know,” she answered, so softly it was arduous to listen to. “Going from here to the bathroom or the door, I get really winded. I don’t know when it’s going to be my last breath.”
Dickens, a lung most cancers survivor, lives in central Harlem, barely getting by. She has severe lung illness and hypertension and suffers common fainting spells. In the previous 12 months, she’s fallen a number of occasions and dropped to 85 kilos, a dangerously low weight.
And she lives alone, with none assist — a extremely perilous state of affairs.
Across the nation, about 2 million adults 65 and older are utterly or principally homebound, whereas a further 5.5 million seniors can get out solely with important issue or help. This is nearly certainly an undercount, for the reason that information is from greater than a dozen years in the past.
It’s a inhabitants whose numbers far exceed these dwelling in nursing properties — about 1.2 million — and but it receives a lot much less consideration from policymakers, legislators, and lecturers who research growing older.
Consider some eye-opening statistics about utterly homebound seniors from a research printed in 2020 in JAMA Internal Medicine: Nearly 40% have 5 or extra power medical circumstances, equivalent to coronary heart or lung illness. Almost 30% are believed to have “probable dementia.” Seventy-seven % have issue with not less than one day by day process equivalent to bathing or dressing.
Almost 40% dwell by themselves.
That “on my own” standing magnifies these people’ already appreciable vulnerability, one thing that grew to become acutely apparent through the covid-19 outbreak, when the variety of sick and disabled seniors confined to their properties doubled.
“People who are homebound, like other individuals who are seriously ill, rely on other people for so much,” stated Katherine Ornstein, director of the Center for Equity in Aging on the Johns Hopkins School of Nursing. “If they don’t have someone there with them, they’re at risk of not having food, not having access to health care, not living in a safe environment.”
Research has proven that older homebound adults are much less prone to obtain common main care than different seniors. They’re additionally extra prone to find yourself within the hospital with medical crises that may have been prevented if somebody had been checking on them.
To higher perceive the experiences of those seniors, I accompanied Gliatto on some house visits in New York City. Mount Sinai’s Visiting Doctors Program, established in 1995, is among the oldest within the nation. Only 12% of older U.S. adults who not often or by no means depart house have entry to this type of home-based main care.
Gliatto and his employees — seven part-time docs, three nurse practitioners, two nurses, two social staff, and three administrative staffers — serve about 1,000 sufferers in Manhattan annually.
These sufferers have sophisticated wants and require excessive ranges of help. In latest years, Gliatto has needed to minimize employees as Mount Sinai has lowered its monetary contribution to this system. It doesn’t flip a revenue, as a result of reimbursement for companies is low and bills are excessive.
First, Gliatto stopped in to see Sandra Pettway, 79, who by no means married or had youngsters and has lived by herself in a two-bedroom Harlem condo for 30 years.
Pettway has extreme spinal issues and again ache, in addition to Type 2 diabetes and melancholy. She has issue shifting round and barely leaves her condo. “Since the pandemic, it’s been awfully lonely,” she instructed me.
When I requested who checks in on her, Pettway talked about her next-door neighbor. There’s nobody else she sees repeatedly.
Pettway instructed the physician she was more and more apprehensive about an upcoming spinal surgical procedure. He reassured her that Medicare would cowl in-home nursing care, aides, and bodily remedy companies.
“Someone will be with you, at least for six weeks,” he stated. Left unsaid: Afterward, she can be on her personal. (The surgical procedure in April went properly, Gliatto reported later.)
The physician listened fastidiously as Pettway talked about her reminiscence lapses.
“I can remember when I was a year old, but I can’t remember 10 minutes ago,” she stated. He instructed her that he thought she was managing properly however that he would organize testing if there was additional proof of cognitive decline. For now, he stated, he’s not notably nervous about her capability to handle on her personal.
Several blocks away, Gliatto visited Dickens, who has lived in her one-bedroom Harlem condo for 31 years. Dickens instructed me she hasn’t seen different folks repeatedly since her sister, who used to assist her out, had a stroke. Most of the neighbors she knew properly have died. Her solely different shut relative is a niece within the Bronx whom she sees about as soon as a month.
Dickens labored with special-education college students for many years in New York City’s public colleges. Now she lives on a small pension and Social Security — an excessive amount of to qualify for Medicaid. (Medicaid, this system for low-income folks, pays for aides within the house. Medicare, which covers folks over age 65, doesn’t.) Like Pettway, she has solely a small mounted earnings, so she will’t afford in-home assist.
Every Friday, God’s Love We Deliver, a company that prepares medically tailor-made meals for sick folks, delivers per week’s price of frozen breakfasts and dinners that Dickens reheats within the microwave. She virtually by no means goes out. When she has power, she tries to do a little bit of cleansing.
Without the continued consideration from Gliatto, Dickens doesn’t know what she’d do. “Having to get up and go out, you know, putting on your clothes, it’s a task,” she stated. “And I have the fear of falling.”
The subsequent day, Gliatto visited Marianne Gluck Morrison, 73, a former survey researcher for New York City’s personnel division, in her cluttered Greenwich Village condo. Morrison, who doesn’t have any siblings or youngsters, was widowed in 2010 and has lived alone since.
Morrison stated she’d been feeling dizzy over the previous few weeks, and Gliatto gave her a fundamental neurological examination, asking her to observe his fingers together with her eyes and contact her fingers to her nostril.
“I think your problem is with your ear, not your brain,” he instructed her, describing signs of vertigo.
Because she had extreme wounds on her toes associated to Type 2 diabetes, Morrison had been getting house well being look after a number of weeks via Medicare. But these companies — assist from aides, nurses, and bodily therapists — had been as a consequence of expire in two weeks.
“I don’t know what I’ll do then, probably just spend a lot of time in bed,” Morrison instructed me. Among her different medical circumstances: congestive coronary heart failure, osteoarthritis, an irregular heartbeat, power kidney illness, and melancholy.
Morrison hasn’t left her condo since November 2023, when she returned house after a hospitalization and several other months at a rehabilitation heart. Climbing the three steps that lead up into her condo constructing is just too arduous.
“It’s hard to be by myself so much of the time. It’s lonely,” she instructed me. “I would love to have people see me in the house. But at this point, because of the clutter, I can’t do it.”
When I requested Morrison who she feels she will depend on, she listed Gliatto and a psychological well being therapist from Henry Street Settlement, a social companies group. She has one shut good friend she speaks with on the cellphone most nights.
“The problem is I’ve lost eight to nine friends in the last 15 years,” she stated, sighing closely. “They’ve died or moved away.”
Bruce Leff, director of the Center for Transformative Geriatric Research on the Johns Hopkins School of Medicine, is a number one advocate of home-based medical care. “It’s kind of amazing how people find ways to get by,” he stated after I requested him about homebound older adults who dwell alone. “There’s a significant degree of frailty and vulnerability, but there is also substantial resilience.”
With the speedy growth of the growing older inhabitants within the years forward, Leff is satisfied that extra sorts of care will transfer into the house, every little thing from rehab companies to palliative care to hospital-level companies.
“It will simply be impossible to build enough hospitals and health facilities to meet the demand from an aging population,” he stated.
But that shall be difficult for homebound older adults who’re on their very own. Without on-site household caregivers, there could also be nobody round to assist handle this home-based care.
KFF Health News is a nationwide newsroom that produces in-depth journalism about well being points and is among the core working packages at KFF—an impartial supply of well being coverage analysis, polling, and journalism. Learn extra about KFF.
USE OUR CONTENT
This story may be republished without spending a dime (details).