Seven years in the past, Robert Kerley, who makes his dwelling as a truck driver, was loading drywall when a gust of wind knocked him off the trailer. Kerley fell 14 toes and damage his again.
For ache, a sequence of docs prescribed him quite a lot of opioids: Vicodin, Percocet and OxyContin.
In lower than a 12 months, the 45-year-old from Federal Heights, Colo., stated he was hooked. “I spent most of my time high, laying on the couch, not doing nothing, falling asleep everywhere,” he stated.
Kerley misplaced weight. He misplaced his job. His relationships along with his spouse and youngsters suffered. He remembers when he hit all-time low: One evening hanging out in a good friend’s basement, he drank three beers, and the alcohol reacted with an opioid.
“I was taking so much morphine that I [experienced] respiratory arrest,” Kerley stated. “I stopped breathing.”
An ambulance arrived, and EMTs administered the overdose reversal drug naloxone. Kerley was later hospitalized. As the daddy of a 12-year-old boy, he knew he wanted to show issues round. That’s when he signed up for Kaiser Permanente‘s built-in ache service. (Kaiser Health News shouldn’t be affiliated with Kaiser Permanente.)
“After seven years of being on narcotics and in a spiral downhill, the only thing that pulled me out of it was going to this class,” he stated. “The only thing that pulled me out of it was doing and working the program that they ask you to work.”
Email Sign-Up
Subscribe to KHN’s free Morning Briefing.
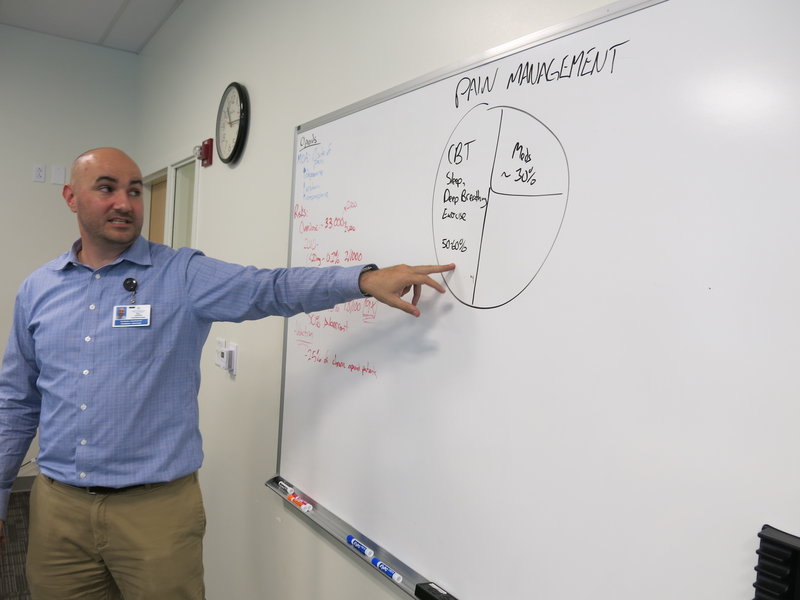
The program he refers to is an eight-week course, out there to Kaiser Permanente members in Colorado for $100. It’s designed to teach high-risk opioid sufferers about ache administration. A current class met at Kaiser’s Rock Creek medical workplaces in Lafayette, Colo., a city east of Boulder. Will Gersch, a medical pharmacy specialist, taught a number of sufferers studying to battle dependancy the science behind pharmaceuticals.
“So, basically the overarching message here is the higher the dose of the opioids, the higher the risk,” he advised the group, as he jotted numbers on a whiteboard. “If you’re over these two doses, that’s a risk factor.”
Amanda Bye, a medical psychologist, works as a part of an built-in medical staff to deal with individuals with continual ache. (John Daley/Colorado Public Radio)
Upstairs, Gersch’s colleague Amanda Bye, a medical psychologist, highlighted a key component of this system: It’s built-in. For affected person care, there’s a physician, a medical pharmacist, two psychological well being therapists, a bodily therapist and a nurse — all on one flooring. Patients can meet with this staff, both abruptly or in teams, however they don’t have to take care of a sequence of referrals and appointments in numerous services. A spokesperson for Kaiser Permanente stated researchers tracked greater than 80 sufferers over the course of a 12 months and located the group’s emergency room visits decreased 25 p.c. Inpatient admissions dropped 40 p.c, and sufferers’ opioid use went approach down.
“We brought in all these specialists. We all know the up-to-date research of what’s most effective in helping to manage pain,” Bye stated. “And that’s how the program got started.”
Bye stated the staff helps sufferers use options like train, meditation, acupuncture and mindfulness. Some sufferers, although, do must go to the chemical dependency unit for medication-assisted remedy for his or her opioid dependancy. Benjamin Miller is an skilled on built-in care with the nationwide basis Well Being Trust. Kaiser is heading in the right direction, he stated.
“The future of health care is integrated and, unfortunately, our history is very fragmented, and we’re just now catching up to developing a system of care that meets the needs of people,” he stated.
Similar initiatives in California confirmed a discount within the variety of prescriptions and tablets per affected person, stated Dr. Kelly Pfeifer, director of high-value care on the California Health Care Foundation. Her group launched case studies of three applications much like Kaiser’s Colorado program. (Kaiser Health News produces California Healthline, an editorially impartial publication of the California Health Care Foundation.)
“We’ve seen great success with these models that are integrating complementary therapy, physical therapy, behavioral health and medical care,” Pfeifer stated. A key technique is to steadily lower the quantity of opioids a affected person takes, quite than reduce them off earlier than they’re prepared. “It works so much better when the patients have access to these complementary therapies,” she stated. “And it works even better when those complementary therapies are part of an integrated team.”
But it may be troublesome to implement universally. One problem is scale: Big programs like Kaiser Permanente have ample sources and sufficient sufferers to take the time work. Another situation is fee. Some insurers gained’t pay for some various remedies; others have separate fee streams for various sorts of care.
“Frequently, behavioral health and medical health are paid for by entirely different systems,” Pfeifer stated.
Robert Kerley is recovering from an opioid dependancy with assist from Kaiser Permanente’s ache administration program in Colorado. (John Daley/Colorado Public Radio)
The want for applications like Kaiser’s is pressing. In 2016, a document 912 individuals died from an overdose in Colorado, in keeping with data recently released by the state health department. Of these, 300 individuals died from an opioid overdose. Opioid use usually results in an dependancy to heroin, which claimed one other 228 lives final 12 months within the state. Those two causes collectively now rival the variety of deaths from automobile accidents within the state.
Colorado faces a extreme scarcity of remedy choices. Making issues worse, the state’s largest substance abuse remedy supplier, Arapahoe House, decided to close as of Jan. 2.
Kaiser’s built-in ache service has given some sufferers a second likelihood.
Robert Kerley, now a veteran of this system, lately shared his story with different sufferers. “I got my life back. I can sleep. I can eat. I can enjoy things,” Kerley advised them.
To deal with ache, Kerley begins his morning with stretching and a model of tai chi that he calls “my chi.” He practices deep respiration. His recommendation to others affected by ache or dependancy?
“Do whatever it takes to walk away from it, like no matter what,” Kerley stated. “Trust me, it gets better. It gets 100 percent better than where you’re at right now.”
Better for Kerley means his relationships along with his household have improved. And he’s again at work, as soon as once more in a position to make a dwelling as a truck driver.
This story is a part of a reporting partnership with NPR, Colorado Public Radio and Kaiser Health News.
Related Topics Public Health States Colorado Opioids Substance Abuse