Jordan Rau, Kaiser Health News
On orders from Congress, Medicare is easing up on its annual readmission penalties on a whole bunch of hospitals serving probably the most low-income residents, information launched final week present.
Since 2012, Medicare has punished hospitals for having too many sufferers find yourself again of their care inside a month. The authorities estimates the hospital trade will lose $566 million within the newest spherical of penalties that may stretch over the following 12 months. The penalties are a signature a part of the Affordable Care Act’s effort to encourage higher care.
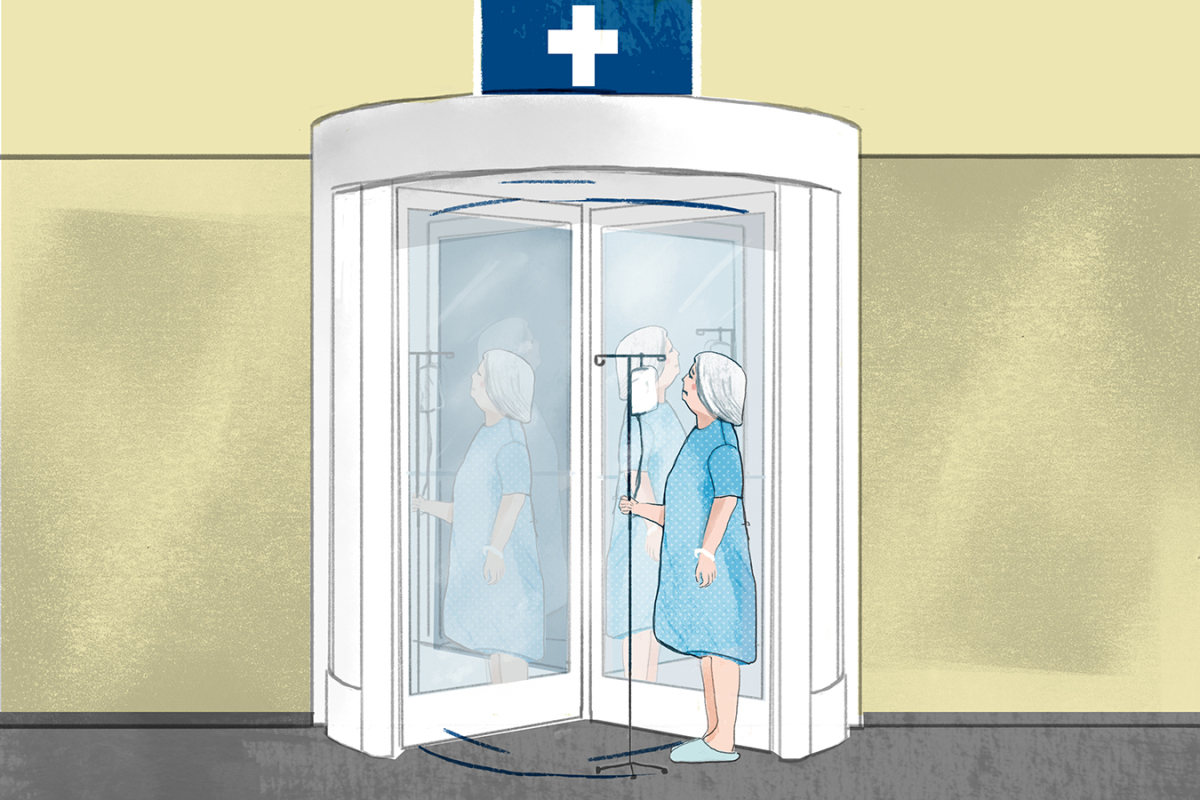
But beginning subsequent month, lawmakers mandated that Medicare take note of a long-standing grievance from safety-net hospitals. They have argued that their sufferers usually tend to undergo problems after leaving the hospital through no fault of the institutions, however moderately as a result of they can’t afford drugs or don’t have common medical doctors to observe their recoveries. The Medicare sanctions have been particularly painful for this class of hospitals, which regularly battle to remain afloat as a result of so lots of their sufferers carry low-paying insurance coverage or none in any respect.
In a major change to its analysis, the federal Centers for Medicare & Medicaid Services (CMS) this yr ceased judging every hospital towards all others. Instead, it assigned hospitals to 5 peer teams of services with related proportions of low-income sufferers. Medicare then in contrast every hospital’s readmission charges from July 2014 via June 2017 towards the readmission charges of its peer group throughout these three years to find out in the event that they warranted a penalty and, in that case, how a lot it ought to be.
The broader subject is whether or not medical suppliers that serve the poor might be pretty judged towards people who take care of the prosperous. This has been a seamless subject of rivalry as the federal government seeks to precisely measure well being care high quality. It is especially a priority in efforts to think about affected person outcomes in setting pay charges for medical doctors, nursing properties, hospitals and different suppliers.
Overall, Medicare will dock funds to 2,599 hospitals — greater than half within the nation— all through fiscal yr 2019, which begins Oct. 1, a Kaiser Health News evaluation of the information discovered. The harshest penalty is three % decrease reimbursements for each Medicare affected person discharged in fiscal yr 2019. The variety of hospitals and the typical penalty — zero.7 % of every cost — are virtually the identical as final yr.
But the brand new methodology shifted the burden of these punishments. Penalties towards safety-net hospitals will drop by a fourth on common from final yr, the evaluation discovered.
“It’s pretty clear they were really penalizing those institutions more than they needed to,” mentioned Dr. Atul Grover, govt vp of the Association of American Medical Colleges. “It’s definitely a step in the right direction.”
(Story continues under. Trouble viewing this desk? Download the info here.)
Safety-net hospitals that may see their penalties minimize by half or extra embody many city establishments, akin to Sutter Health’s Alta Bates Summit Medical Center in Oakland, Calif.; Providence Hospital in Washington, D.C.; and Hurley Medical Center in Flint, Mich. Sixty-five safety-net hospitals — together with Franklin Medical Center in Winnsboro, La., Astria Toppenish Hospital in Toppenish, Wash., and Emanuel Medical Center in Swainsboro, Ga. — that had been penalized final yr escaped punishment totally this yr.
Conversely, the typical penalty for the hospitals with the fewest low-income sufferers will rise from final yr, the evaluation discovered.
Before this system started, roughly 1 in 5 Medicare beneficiaries have been readmitted inside a month. Hospitals have been paid the identical quantity no matter how their sufferers fared after being discharged. In reality, a readmission was financially advantageous as hospitals can be paid for the second hospital keep, even when it might need been avoidable.
Since the sanctions started, Medicare has evaluated every year charges for readmitted sufferers who had initially been handled for coronary heart failure, coronary heart assaults and pneumonia. And it has lowered its funds to greater than half of hospitals based mostly on these charges. The evaluations have since expanded to cowl power lung illness, hip and knee replacements and coronary artery bypass graft surgical procedures.
Medicare counts sufferers who returned to a hospital inside 30 days, even when it’s a totally different hospital than the one which initially handled them. The penalty is utilized to the primary hospital.
Medicare exempts hospitals with too few instances, these serving veterans, kids and psychiatric sufferers, and critical-access hospitals, that are the one hospitals inside attain of some sufferers. In addition, Maryland hospitals are excluded as a result of Congress lets that state set its personal guidelines on the way it distributes Medicare cash.
(Story continues under.)
In its revised methodology this yr, Medicare distinguished hospitals that serve a excessive proportion of low-income sufferers by taking a look at how lots of the hospital’s Medicare sufferers have been additionally eligible for Medicaid, the state-federal program for the poor. American Hospital Association officers say that whereas they thought-about this an enchancment, it isn’t an ideal reflection of poor sufferers. For one factor, they are saying, hospitals in states with extra restrictive Medicaid protection don’t seem via this formulation to have as difficult affected person populations as do hospitals in states with increased Medicaid eligibility.
Akin Demehin, the affiliation’s director of high quality coverage, mentioned CMS may contemplate linking its information to Census information that present revenue and training degree of sufferers.
“It might give you a more precise adjuster,” he mentioned.
The hospital trade stays essential of the general program, saying that stripping hospitals of income due to poor efficiency solely makes it tougher for them to take care of sufferers.
Congress’ Medicare Payment Advisory Commission in June concluded that the penalties from earlier years efficiently pressured hospitals to cut back the numbers of returning sufferers — and helped save Medicare about $2 billion a yr.
In its evaluation of the strategy’s effectiveness, Congress’ advisory fee rejected a number of the hospital industries’ complaints about Medicare’s Hospital Readmissions Reduction Program: that hospitals could have tried to get around the penalties by preserving sufferers underneath “observation status” and that discouraging rehospitalizations could have led to extra deaths.
The fee discovered that between 2010 and 2016 readmission charges fell by three.6 proportion factors for coronary heart assaults, three proportion factors for coronary heart failure and a couple of.three proportion factors for pneumonia. At the identical time, readmissions attributable to circumstances that don’t issue into the penalties fell on common 1.four proportion factors, indicating hospitals have been specializing in decreasing pointless readmissions that would damage them financially.
The fee wrote: “We conclude that the [penalties] contributed to a significant decline in readmission rates without causing a material increase in ED [emergency department] visits, a material increase in observation stays, or a net adverse effect on mortality rates.”
This fall, Medicare will assault the readmissions from one other angle by issuing penalties on skilled nursing facilities that ship just lately discharged residents again to the hospital too steadily.
KHN’s protection associated to getting old and bettering care of older adults is supported partially by The John A. Hartford Foundation.
Kaiser Health News (KHN) is a nationwide well being coverage information service. It is an editorially impartial program of the Henry J. Kaiser Family Foundation which isn’t affiliated with Kaiser Permanente.