Use Our Content This story might be republished without cost (details).
Public well being officers in California’s state capital area introduced this week they’ve stopped tracing the contacts of sufferers identified with the novel coronavirus. They’ve additionally ceased recommending quarantines for residents uncovered to individuals confirmed to have the virus.
It was a grim recognition of the virus’ infiltration — and is one more signal of the detrimental results of a scarcity of functionality within the U.S. to check individuals for the lethal coronavirus because it continues to unfold.
“The reason we have to move on is because testing did not occur. We’re still able to do about 20 tests a day,” stated Dr. Peter Beilenson, director of Sacramento County’s Department of Health Services. “If you really wanted to quarantine and contain the situation, you would have wanted to know who was positive and quarantine them. Because we never had the tests, it’s kind of a moot point, and the horse is out of the barn.”
Sacramento County — which as of Friday had 17 confirmed instances of COVID-19, together with one demise — as an alternative has begun advising residents to make use of so-called social distancing measures as a major response. That consists of asking individuals and companies to cancel massive gatherings, warning older individuals and people with power circumstances to keep away from crowds, and begging most of the people to apply good hygiene.
Email Sign-Up
Subscribe to KHN’s free Morning Briefing.
The transfer is a part of a shift from containment — the place the objective is to trace each case of the illness and finish its unfold — to mitigation, which focuses on defending essentially the most susceptible from the consequences of a illness that’s already widespread all through the group. County residents with any kind of sickness are being requested to self-isolate till a number of days after signs resolve.
“Our goal is to be much more surgical in our approach to prevent the spread to seniors,” Beilenson stated.
Sacramento County’s troublesome determination to alter course comes even because the director-general of the World Health Organization has stated that it’s “wrong and dangerous” for international locations to shift from containment to mitigation at this level within the pandemic. “Countries that decide to give up on fundamental public health measures may end up with a larger problem, and a heavier burden on the health system that requires more severe measures to control,” stated Dr. Tedros Adhanom Ghebreyesus.
The U.S. has not made that shift as an entire, however specialists say it’s regarding that some areas of the nation have needed to transfer away from the essential public well being protocols of contact tracing and quarantine in response to the federal authorities’s botched rollout of coronavirus take a look at kits.
“Every tool should still be on the table,” stated Dr. Ashish Jha, a professor of worldwide well being at Harvard University. “We should not give up on containment. It’s a very big challenge ahead, but I feel like we are starting to make progress as a country, and if we do an all-of-the-above strategy, there’s a pretty good chance we’re going to get through this without too much harm to our population.”
King County in Washington state, which has been an early epicenter for the virus within the U.S., shifted from contact tracing as properly, however nonetheless requires a 14-day quarantine for individuals who have been uncovered to somebody with the virus. Yolo and Placer counties in California even have shifted to a mitigation strategy, although the main points fluctuate.
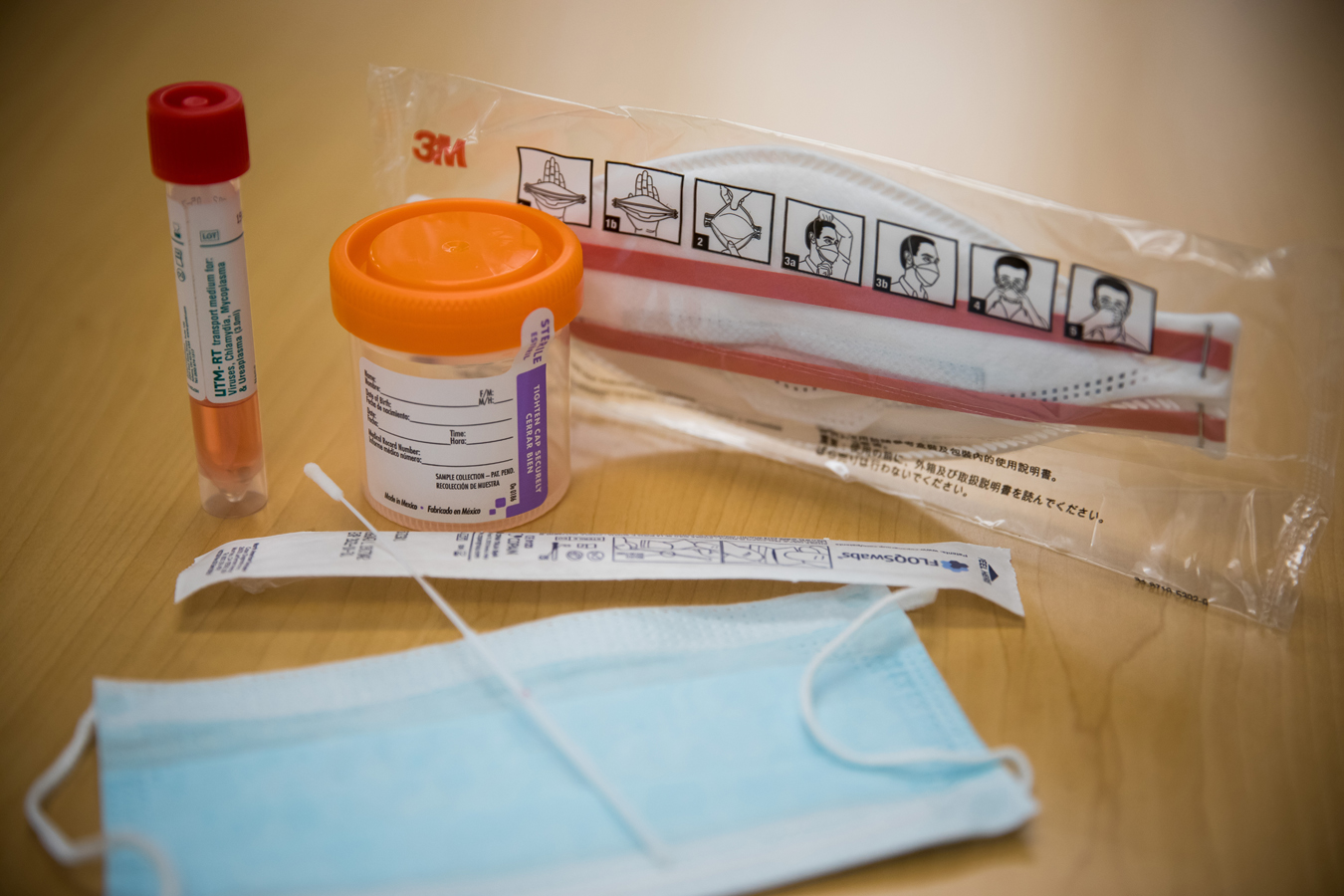
The nation’s response to COVID-19 has been hampered by a spread of issues with the federal authorities’s checks. Kits designed and launched by the federal Centers for Disease Control and Prevention initially didn’t work; a slim testing protocol meant it possible took weeks for some communities to know that the virus was circulating regionally; industrial labs started testing solely this week, and it may possibly take greater than 4 days for these outcomes to return again.
President Donald Trump promised once more Friday that the U.S. is ramping up efforts to companion with non-public firms on take a look at manufacturing. But entry to testing stays sharply restricted, and varies broadly from state to state and county to county. As of Friday, the variety of U.S. residents examined stood within the hundreds. By distinction, South Korea has been testing 10,000 individuals a day for weeks.
The restricted testing capability in California is a urgent concern, Gov. Gavin Newsom stated throughout a information convention Thursday. The variety of take a look at kits is insufficient, the state faces a scarcity of reagents wanted to run the checks, and plenty of counties can’t but run their very own checks. He stated the state will contract with industrial labs to cope with anticipated backlogs.
Even susceptible individuals who had contact with individuals recognized to have the virus can’t get rapid testing. Two days after a resident at a Carlton Senior Living facility turned Sacramento County’s first COVID-19 demise, Dr. Mark Ghaly, secretary of California’s Health and Human Services Agency, stated that every one residents have been being monitored. But they hadn’t all been examined for the virus. “We are working to make sure that those who need testing, that we have it available,” he advised reporters, “and are working with the facility to determine who will get tested very soon.”
Containment requires each testing to seek out out who has the virus, and the manpower to observe up on the outcomes — and state and native public well being departments lack enough sources for each, stated Dr. Cyrus Shahpar, former group lead of the worldwide speedy response group on the CDC.
In Wuhan, China, for instance, 1,800 teams of epidemiologists, every manufactured from up of 5 individuals, traced tens of hundreds of contacts every day. “We would never be able to do that. Contact tracing is very resource-intensive,” stated Shahpar. “It’s not like public health departments have 50 standby teams to do this.”
The federal authorities final week allotted $eight billion in emergency funding for the coronavirus response, however the transfer got here almost two months after the risk emerged, and lengthy after early testing would have helped include the virus. “A lot of parts of the country have already had community transmission. It’s late,” Shahpar stated.
Without the power to check, it’s laborious to know if we’re abandoning containment methods too quickly, stated Alan Melnick, well being officer for Clark County, Washington. During a measles outbreak in 2019, his county was in a position to muster the sources to observe greater than 800 individuals. But throughout that epidemic, they may pull in sources from the surface. Today, few locations have sources to spare. Decades of stagnant budgets have left public well being departments making an attempt to do extra with much less.
“When you’re fighting a war with bubble gum and shoestrings, you’re forced to make difficult decisions,” stated Alex Briscoe, a principal at California Children’s Trust and former director of the Alameda County Health Care Services Agency. “The burden we are placing on an underfunded public health infrastructure is unreasonable and unacceptable.”
Use Our Content This story might be republished without cost (details).
This KHN story first printed on California Healthline, a service of the California Health Care Foundation.
Jenny Gold: [email protected]”>[email protected], @JennyAGold
Anna Maria Barry-Jester: [email protected]”>[email protected], @annabarryjester
Related Topics California Public Health States COVID-19 src=”http://platform.twitter.com/widgets.js” charset=”utf-8″>