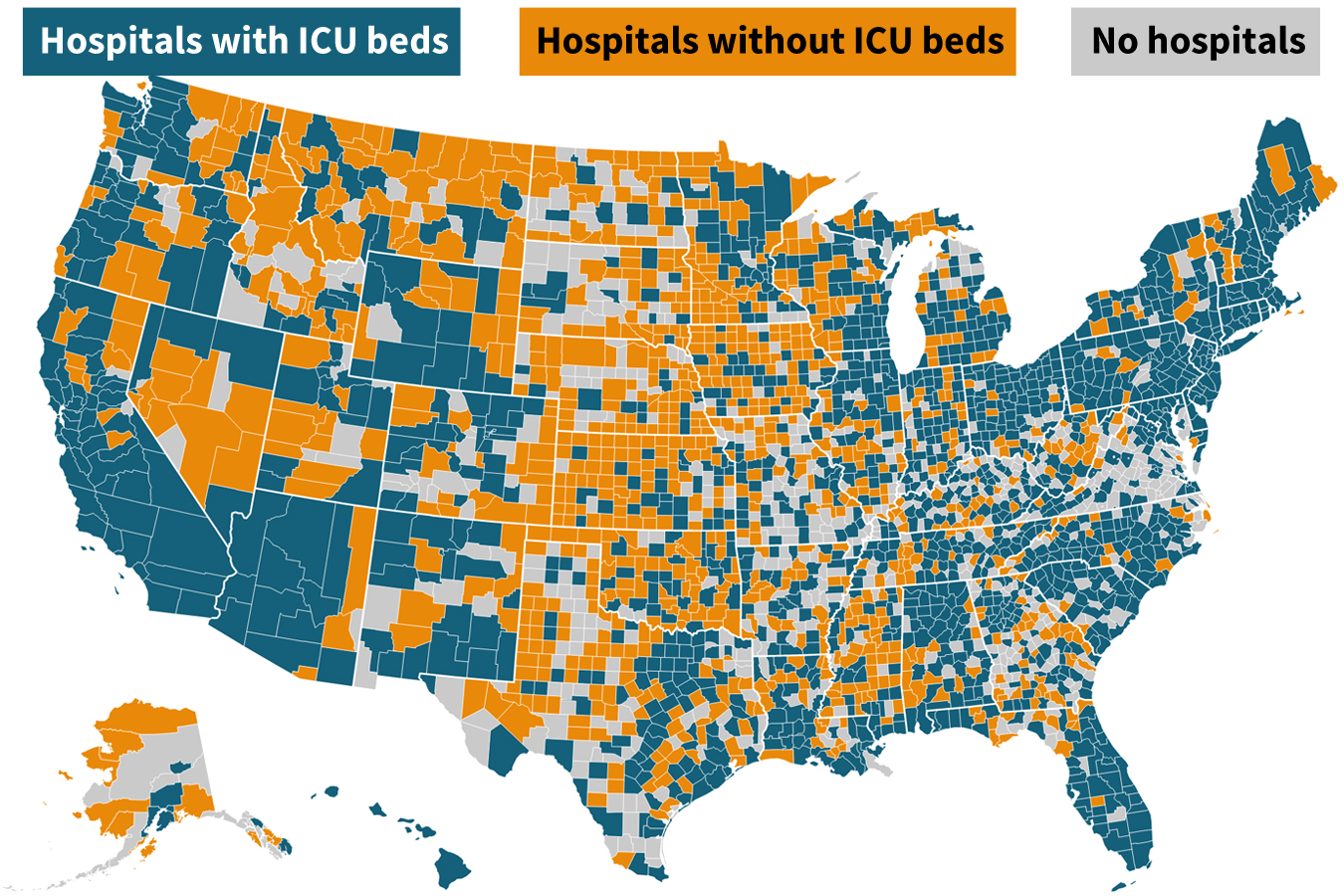
More than half the counties in America don’t have any intensive care beds, posing a specific hazard for greater than 7 million people who find themselves age 60 and up ― older sufferers who face the best danger of great sickness or demise from the speedy unfold of COVID-19, a Kaiser Health News information evaluation reveals.
This story additionally ran on USA Today. This story could be republished totally free (details). Intensive care models have subtle tools, corresponding to bedside machines to observe a affected person’s coronary heart price and ventilators to assist them breathe. Even in communities with ICU beds, the numbers fluctuate wildly ― with some having only one mattress accessible for 1000’s of senior residents, based on the evaluation primarily based on a overview of knowledge hospitals report annually to the federal authorities.
Consider the properties of two midsize cities: The Louisville space of Jefferson County, Kentucky, as an illustration, has one ICU mattress for each 442 individuals age 60 or older, whereas in Santa Cruz, California, that quantity stands at one mattress for each 2,601 residents.
Differences are huge inside every state as properly: San Francisco, with one mattress for each 532 older residents, and Los Angeles, with 847 residents per mattress, each have higher mattress availability than does Santa Cruz.
Even counties that rank within the high 10% for ICU mattress rely nonetheless have as many as 450 older individuals doubtlessly competing for every mattress.
The KHN findings put in stark aid a wrenching problem hospitals in lots of communities — each city and rural ― may face throughout the coronavirus pandemic: deciding learn how to ration scarce assets.
“This is just another example of geography determining access to health care,” Arthur Caplan, a bioethics professor at NYU Langone Medical Center, mentioned when informed of KHN’s findings.
Overall, 18 million individuals stay in counties which have hospitals however no ICU, a few quarter of them 60 or older, the evaluation reveals. Nearly 11 million extra Americans reside in counties with no hospital, some 2.7 million of them seniors.
Dr. Karen Joynt Maddox, a professor at Washington University School of Medicine in St. Louis, mentioned that hospitals with bigger numbers of ICU beds are likely to cluster in higher-income areas the place many sufferers have non-public medical health insurance.
“Hospital beds and ICU beds have cropped up where the economics can support them,” she mentioned. “We lack capacity everywhere, but there are pretty big differences in terms of per capita resources.”
Doctors in rural counties are bracing for the chance they might run out of essential care beds. Northern Light Sebasticook Valley Hospital, in central Maine, has one ventilator and 25 beds. Two of these are “special care” beds that don’t meet full necessities for intensive care however are reserved for the sickest individuals. Such sufferers are sometimes transferred elsewhere, maybe to the town of Bangor, by ambulance or helicopter.
But that might not be potential if COVID-19 surges throughout the state “because they’re going to be hit just as hard if not harder than we will be,” mentioned Dr. Robert Schlager, chief medical officer on the hospital in rural Pittsfield. “Just like the nation, we probably don’t have enough, but we’re doing the best we can.”
Hospitals additionally say they will shortly devise plans to switch circumstances they will’t deal with to different services, although some sufferers could also be too in poor health to danger the transfer.
Certainly, being in a county with few or no ICU beds might not be as dire because it appears if that county abuts one other county with a extra strong provide of such beds.
In Michigan, well being planners have decided that rural counties with few ICU beds, corresponding to Livingston and Ionia, within the central a part of the state, can be served by main services in close by Lansing or Detroit in a significant disaster.
Dr. Peter Graham, govt medical director for Physicians Health Plan in Michigan, is affiliated with Sparrow Health System in Lansing. He is making no assumptions. It’s potential central Michigan may take overflow COVID-19 sufferers from Detroit if that’s the place the illness clusters, he mentioned. Or sufferers may need to be transferred tons of of miles away.
“It’s just obvious people are going to need to move” if native services are overwhelmed, he mentioned. “If we’re able to find a ventilator bed in Indianapolis, in Chicago or Minneapolis or wherever, it is go, get them there!”
Yet consultants warn that even areas comparatively wealthy in ICU beds may very well be overwhelmed with sufferers struggling to breathe, a typical symptom of severely in poor health COVID-19 sufferers.
“No matter how you look at it, the numbers [of ICU beds] are too small,” mentioned Dr. Atul Grover, govt vice chairman of the Association of American Medical Colleges. “It’s scary.”
Lenard Kaye, director of the University of Maine Center on Aging, a state with a big older inhabitants and comparatively few ICU beds, agreed. “The implications are tremendous and very troubling,” he mentioned. “Individuals are going to reach out for help in an emergency, and those beds may well not be available.”
Health staff may must resort to “triaging and tough decisions,” Kaye mentioned, “on who beds are allocated to.”
That concern isn’t misplaced on Linnea Olsen, 60, who has lung most cancers and is aware of she is particularly weak to any respiratory virus.
Olsen worries a few potential scarcity of ventilators and ICU beds, which may lead medical doctors to ration essential care. Given her fragile well being, she fears she wouldn’t make the lower.
“I’m worried that cancer patients will be a low priority,” mentioned Olsen, a mom of three grownup kids, who lives in Amesbury, Massachusetts.
Olsen, who was recognized with lung most cancers virtually 15 years in the past, has survived far longer than most individuals with the illness. She is now being handled with an experimental treatment — which has by no means been examined earlier than in people ― in an early-stage scientific trial. It’s her fourth early scientific trial.
“I’m no longer young, but I still would argue that my life is worthwhile, and my three kids certainly want to keep me around,” she mentioned.
She mentioned she has “fought like hell to stay alive” and worries she gained’t be given a preventing likelihood to outlive COVID-19.
“Those of us with lung cancer are among the most vulnerable,” Olsen mentioned, “but instead of being viewed as someone to be protected, we will be viewed as expendable. A lost cause.”
Overall, 26 million individuals stay in counties with hospitals however no ICU, a few quarter of them older than 60. Nearly 11 million extra Americans reside in counties with no hospital, some 2.7 million of them seniors.
The complete variety of ICU beds nationally varies, relying on which supply is consulted and which beds are counted. Hospitals reported 75,000 ICU beds of their most up-to-date annual monetary experiences to the federal government, however that excludes Veterans Affairs’ services.
The United States has about thrice as many ICU beds per capita as Italy and 10 occasions as many as China, two nations ravaged by COVID-19, based on a brand new report from the Society of Critical Care Medicine. The provide of ventilators additionally exceeds different developed nations, another study found. But as with ICU beds, “there is wide variation [in ventilators available] across states,” the examine discovered.
Many consultants predict that demand could quickly exceed the provision. Over a interval of months, the nation might have 1.9 million ICU beds — 20 occasions the present provide ― to deal with COVID-19 sufferers, based on the American Hospital Association.
Dr. Tia Powell, who co-chaired a 2007 New York State Department of Health group that set tips for rationing scarce ventilators, mentioned stopping wildfire-like unfold of illness is essential to retaining sick sufferers from overcrowding hospitals.
“If it spreads slowly, you’re much less likely to run short of critical supplies,” she mentioned. “If you need all of your ventilators right now, this week, that’s what makes trouble.”
Even slowing the pandemic doesn’t assure hospitals can cope. While some hospitals are planning to deal with sufferers with much less critical sickness in tents, it’s far harder to create intensive care models and even develop present ones, mentioned Dr. Greg Martin, president-elect of the Society of Critical Care Medicine, which represents intensive care medical doctors.
Martin mentioned ventilators should be hooked as much as oxygen and gasoline traces to provide the suitable mixture of air sufferers want. To convert a typical hospital unit to an ICU, “you would literally need to tear down the wall and run the piping in,” he mentioned.
Few areas — corresponding to working rooms, emergency division and models used for post-anesthesia care ― have the hookups wanted, based on Martin.
Intensive care models additionally require specifically skilled medical doctors, nurses and respiratory therapists. While nurses in different areas of the hospital could look after six sufferers, ICU nurses sometimes concentrate on one or two, Martin mentioned.
“Mechanical ventilation of a fragile patient is rather dangerous if provided by someone other than these trained ICU professionals, which is why mechanical ventilation is not typically done outside of the ICU,” the group mentioned.
Bob Atlas, president and CEO of the Maryland Hospital Association, famous that hospitals and authorities officers have been discussing methods to spice up staffing ranges, corresponding to calling on medical doctors with expired medical licenses, or these licensed to apply in different states, to deal with sufferers in viral sizzling spots.
Also up for dialogue: loosening guidelines for “scope of practice,” laws that spell out the duties medical professionals are permitted primarily based on their coaching.
Atlas and others mentioned they hope steps hospitals have taken to liberate beds, corresponding to deferring nonessential surgical procedure, will preserve the system from collapsing.
“It’s not as if every Medicare beneficiary will need an ICU bed,” he mentioned. He additionally mentioned hospitals may wind up treating solely the sickest sufferers.
Greg Burel, the previous director of the Strategic National Stockpile, mentioned he hoped that hospitals missing ICU beds may shortly iron out switch agreements to maneuver critically in poor health sufferers.
“Let’s hope we don’t get there,” he mentioned.
Novant Health Brunswick Medical Center, on North Carolina’s coast, ordered extra ventilators two months in the past in case COVID-19 went world. It has six and expects 4 extra, mentioned Shelbourn Stevens, its president. But it has solely 5 intensive care beds amongst its 74-bed complete.
Drawing on a long time of expertise with emergency care after hurricanes, the hospital’s employees is lowering elective-surgery circumstances and getting ready to quickly enhance screening for the brand new coronavirus.
“I’m very comfortable with our plans right now,” Stevens mentioned. “Disaster planning is in our bones, so to speak. Our team knows how to react.”
But the hospital’s critical-care capability is proscribed. North Carolina’s Brunswick County, the place it’s situated, has one mattress for each 2,436 residents 60 and older. Such a inhabitants may overwhelm the ability in a COVID-19 surge.
If vital, sufferers may very well be transferred to the bigger New Hanover Regional Medical Center, a brief helicopter journey away, in Wilmington, North Carolina, Stevens mentioned. But with 57 intensive care beds, New Hanover County, which incorporates Wilmington, nonetheless ranks within the decrease two-thirds of counties for ICU beds per senior residents.
If the pandemic turns into extreme, no quantity of critical-care beds shall be sufficient, consultants say.
“I liken it to sitting on a Gulf shore when a hurricane is offshore,” mentioned Dr. Graham, from Michigan. “It’s a question of how soon and how hard.”
KHN senior correspondent JoNel Aleccia contributed to this report.
METHODOLOGY
Kaiser Health News evaluated the capability of intensive care unit (ICU) beds across the nation by first figuring out the variety of ICU beds every hospital reported in its most up-to-date monetary price report, filed yearly to the Centers for Medicare & Medicaid Services. KHN included beds reported within the classes of intensive care unit, surgical intensive care unit, coronary care unit and burn intensive care unit.
KHN then totaled the ICU beds per county and matched the information with county inhabitants figures from the Census Bureau’s American Community Survey. KHN centered on the variety of individuals 60 and older in every county as a result of older individuals are thought of the most certainly group to require hospitalization, given their elevated frailty and present well being circumstances in contrast with youthful individuals. For every county, KHN calculated the variety of individuals 60 and older for every ICU mattress. KHN additionally calculated the proportion of county inhabitants who had been 60 or older.
KHN’s ICU mattress tally doesn’t embody Veterans Affairs hospitals, that are positive to play a job in treating coronavirus victims, as a result of VA hospitals don’t file price experiences. The complete variety of the nation’s ICU beds in the associated fee experiences is lower than the quantity recognized by the American Hospital Association’s annual survey of hospital beds, which is the opposite authoritative useful resource on hospital traits. Experts attributed the discrepancies to totally different definitions of what qualifies as an ICU mattress and different components, and informed KHN each sources had been equally credible.