As the variety of COVID-19 sufferers climbs and well being officers hunt for ventilators to deal with them, nursing houses throughout the United States have a cache ― about eight,200 of the lifesaving machines, in accordance with data from the Centers for Medicare & Medicaid Services.
Most of the machines are in use, typically by individuals who’ve suffered a mind damage or stroke. Some of these residents are in a vegetative state and have remained on a ventilator for years.
State officers are working to consolidate ventilators the place they’re most urgently wanted. But thus far, the provision in nursing houses has not drawn the identical consideration.
Or course, commandeering these models would arrange a monumental moral dilemma: Do you take away life help for a long-term nursing care affected person to be able to give a COVID-19 affected person a greater likelihood of survival?
The highest variety of machines, about 2,300, is in California, the place the state has created designated nursing dwelling models for individuals on life help, formally known as subacute models however recognized pejoratively by some medical doctors as “vent farms.” New York has the second most, 1,822, in accordance with state officers.
Already, one nursing dwelling on Long Island has lent a close-by hospital 11 ventilators that weren’t getting used, leaving simply 5 for its residents.
“The hospital came to us last week and asked, ‘Do you have any ventilators?’” the nursing dwelling assistant administrator stated on the situation of anonymity as a result of he was not approved to talk to the information media.
“We left ourselves with the bare minimum,” he stated. In all, three hospitals reached out to the nursing dwelling for ventilators ― it needed to say no to the opposite two.
New York Gov. Andrew Cuomo has announced an executive order that ventilators not in use by hospitals be redeployed to ICUs. And he’s calling within the New York National Guard to facilitate the order. “We know where every ventilator is,” Cuomo stated Sunday.
Nursing dwelling ventilators will not be included in his order, however they’re included within the state’s tally of the machines.
Dr. Michael Kalafer, a pulmonologist and the medical director at two San Diego subacute models, stated he can’t think about taking one in every of his sufferers off a ventilator as a result of it’s wanted for another person.
“I severely doubt we’ll take [a hypothetical] Mrs. Smith off a ventilator because she’s 80 and has been on it for a few years and has not gotten better,” Kalafer stated.
But these are exactly the choices bioethicists are being requested to weigh in on because the nation confronts the crush of COVID-19 sufferers overwhelming the well being care system.
And in some circumstances, states have already decided to offer people who find themselves severely brain-injured a decrease precedence with regards to entry to ventilators. Disability advocates oppose such tips and filed complaints with the Department of Health and Human Services final month, in accordance with ProPublica. And though states and well being associations can draw up suggestions, they don’t seem to be legally binding.
“From an ethical point of view, for people who are not conscious, if it’s a matter of removing people from a [ventilator] who are not going to recover, I think it’s a hard decision, but one that in an emergency has to be made,” stated Ronald Bayer, a professor of sociomedical sciences on the Mailman School of Public Health at Columbia University.
Bayer has been a member of the World Health Organization and in 2011 served on an ethics subcommittee that suggested the Centers for Disease Control and Prevention on the allocation of ventilators within the occasion of a extreme pandemic.
He and several other different ethicists stated these selections shouldn’t be made on the bedside however by triage committees or individuals in supervisory roles. And the rules must be uniform and clear. That’s why the CDC, the state of New York and medical associations just like the American College of Chest Physicians have drafted moral suggestions for deciding find out how to ration lifesaving gear like ventilators within the occasion of a pandemic.
The California Department of Public Health in 2008 launched guidelines to follow during a health care surge: They don’t particularly tackle ventilator allocation, however fairly assets basically. Doctors ought to think about the chance of survival and alter within the high quality of life versus the flexibility to pay or the notion of an individual’s price when there will not be sufficient medical assets to deal with everybody in want.
When the New York State Task Force on Life and the Law up to date its ventilator allocation tips in 2015, it thought-about the query of withdrawing ventilators from nursing dwelling residents, or power ventilator sufferers, to save lots of the lives of those that develop critically in poor health throughout a pandemic.
“Are we comfortable sacrificing this group in exchange for saving more lives?” requested Stuart Sherman, the chief director of the duty drive on the time.
That query drew a lot debate, however the group finally determined that “chronic” vent sufferers shouldn’t be included within the pool when contemplating find out how to allocate ventilators throughout a pandemic. The process drive does advocate prioritizing ventilator remedy based mostly on who’s more likely to survive utilizing a SOFA ― Sequential Organ Failure Assessment ― rating.
Cuomo, whose day by day televised information conferences have made “ventilators” a family phrase, will not be making selections based mostly on these tips. The process drive report will not be a binding coverage doc, in accordance with a spokesperson from the governor’s workplace.
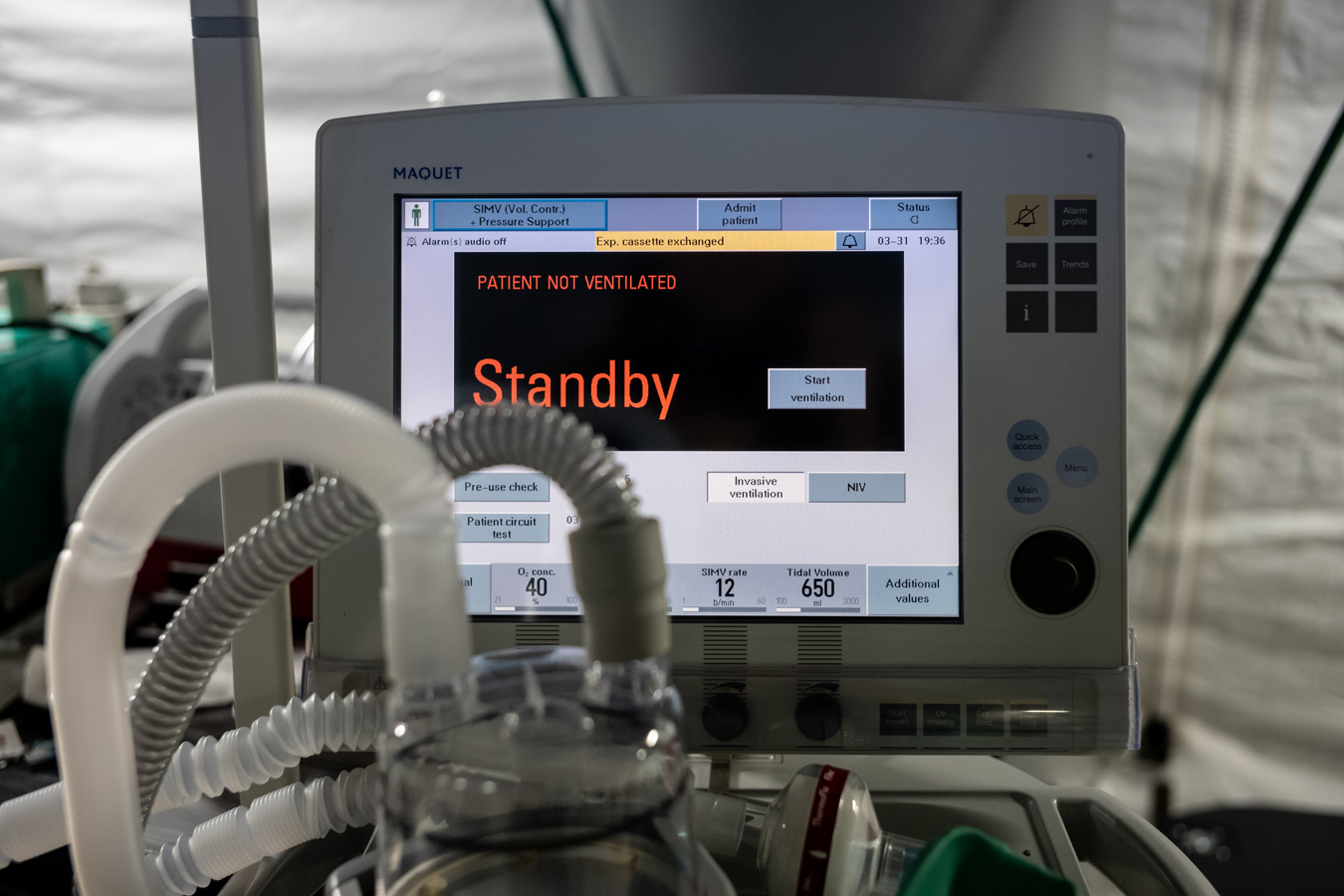
In the U.S., there are about 62,000 “full-featured ventilators,” the sort wanted to deal with probably the most extreme circumstances of COVID-19. An extra 10,000 to 20,000 ventilators are within the authorities’s National Strategic Stockpile, and 98,000 primary fashions, the sort typically in nursing houses, exist that could possibly be utilized in a disaster.
In the only phrases, ventilators push oxygen into the lungs. The machines in ICUs are extra highly effective and have higher monitoring techniques than these in a nursing dwelling.
Kalafer’s sufferers want ventilators to do the work for respiratory muscle tissue. He stated they could possibly be utilized in a pinch in the course of the pandemic. But the true problem is discovering sufficient employees educated to function and monitor the machines.
Meanwhile, a gaggle of bioethicists, physicians and public well being specialists are recommending that in a scarcity, well being care employees might disconnect individuals from ventilators who’ve little or no likelihood of restoration to place them in service of those that do.
The suggestion is the primary of six listed in an article revealed within the New England Journal of Medicine final month.
It didn’t think about the individuals who’ve been on vents long run.
“Honestly, before you emailed me, I thought about those patients but never thought about the actual number and how important that might be,” stated Dr. James Phillips, one of many paper’s authors and chief of catastrophe and operational medication at George Washington University Hospital.
“For patients who have devastating neurological injury and are deemed to never recover and who require ventilation for the rest of their lives, I think it’s an ethical conversation to have with those families to determine if it’s a more appropriate use of resources,” Phillips stated.
One ventilator can save a number of lives. The common time an individual sick with COVID-19 who wanted a ventilator was 11 days, in accordance with an NEJM article that checked out critically in poor health sufferers within the Seattle area. Using that quantity, eight individuals might doubtlessly be saved over three months.
It is an particularly complicated ethical dilemma when contemplating the withdrawal of therapy from somebody who has lived a number of years on a ventilator, stated Govind Persad, an assistant professor on the University of Denver Sturm College of Law and one of many authors of the NEJM paper.
Persad provided a hypothetical state of affairs.
“A 78-year-old grandmother has been on ventilator support for 5 years in a subacute facility and is expected to remain on it for the foreseeable future. Covid-19 has reached a senior apartment complex nearby, and doctors are looking everywhere for more ventilators,” Persad wrote.
“They think one more ventilator would give them a chance of saving another 78-year-old grandmother in the senior apartments who is growing worse with viral pneumonia, and, once she is off the ventilator, to save some of her neighbors, who are not yet sick but who they expect to be sick in a few weeks.”
Who will get the ventilator?
Persad advised it ought to go to the grandmother within the senior residences as a result of she is more likely to want much less time on the ventilator, enabling the ventilator for use to save lots of her neighbors later.
As he put it: “We save her in order to save more lives, not because of quality-of-life judgments.”
The real-life resolution is extra problematic and heart-wrenching.
Nancy Curcio’s daughter Maria, who was born with a disabling type of cerebral palsy, was on a ventilator as an grownup in San Diego for about three months in 2004. She was finally weaned off the machine however lived the rest of her life in a nursing dwelling with a respiration and feeding tube, unable to stroll or discuss. She died in 2017 at age 57.
“I would be very upset if a doctor said I have to take her ventilator away for someone to live,” Curcio stated. “But I can understand in triage this is what a doctor has to do. Would I like it? No. I would want to run away with the ventilator.”