This story is a part of a partnership that features NPR and Kaiser Health News.
This story may be republished at no cost (details).
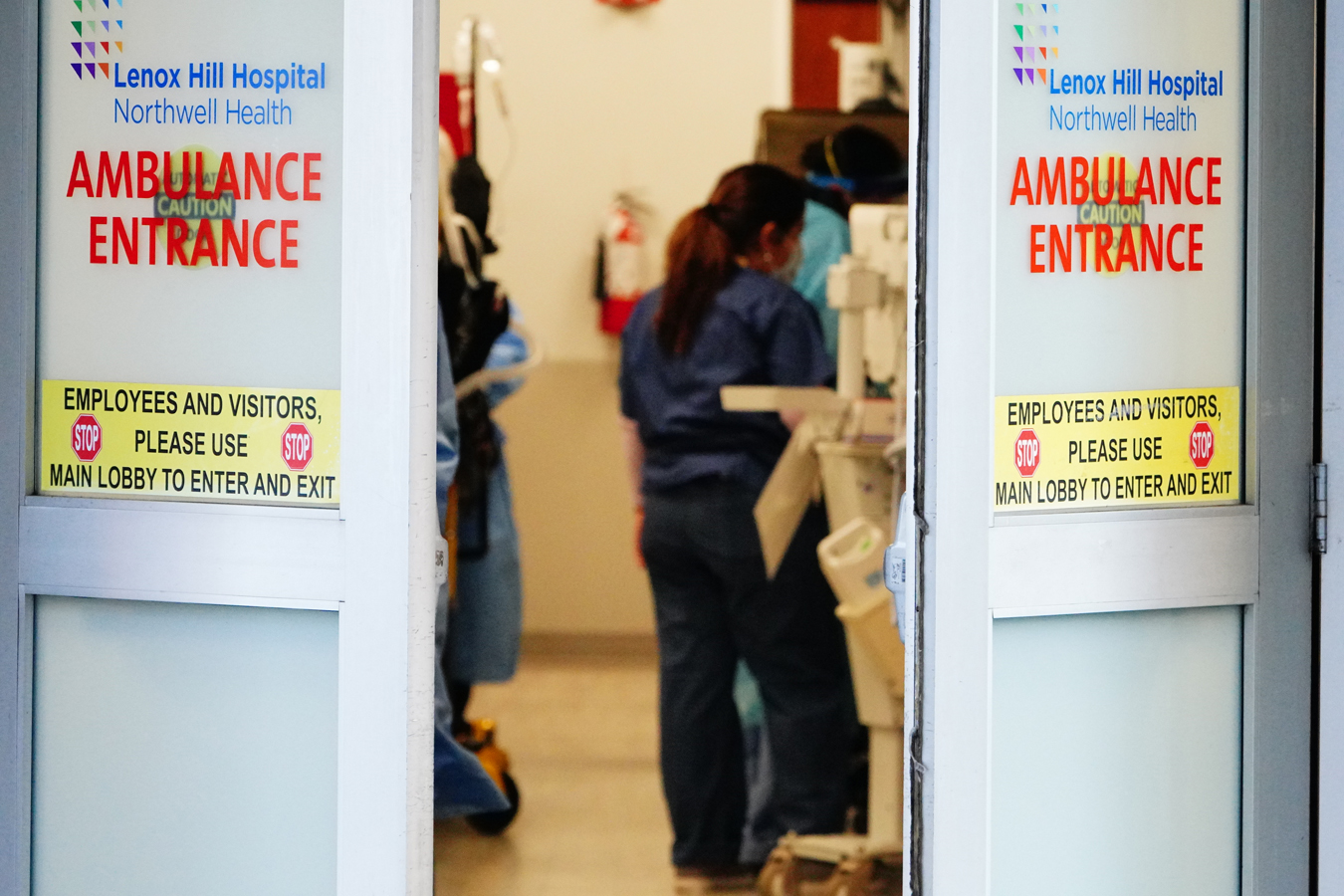
At one New York City hospital, a health care provider’s used masks tore as she carried out CPR on her contaminated affected person.
In Seattle, a nurse compares strolling into her intensive care unit to bathing in COVID-19.
And in St. Louis, a nurse slips her used N95 masks right into a paper bag on the finish of her shift and prays it’s disinfected correctly.
These are scenes enjoying out in hospitals throughout the nation, based mostly on interviews with over a dozen residents, medical doctors and nurses who go into work day-after-day feeling unprotected from the illness they’re imagined to deal with.
Nearly a month into the declared pandemic, some well being care staff say they’re exhausted and burning out from the stress of treating a stream of critically in poor health sufferers in an more and more overstretched well being care system. Many are questioning how lengthy they’ll threat their very own well being. Some are falling sick themselves, and even dying. In many hospitals, the pandemic has reworked emergency rooms and upended protocols and precautions that staff beforehand took as a right.
“It’s like walking into Chernobyl without any gear,” stated Jacklyn, an ER physician at a New York City hospital who requested to go by her center identify for worry of being fired over talking out.
At her hospital, 90% of sufferers have COVID-19, however well being care staff get just one N95 masks each 5 days.
“We’re constantly breathing in everything that’s aerosolized because of all of the procedures that we’re doing,” the New York City physician stated.
Email Sign-Up
Subscribe to KHN’s free Morning Briefing.
Coronavirus can unfold simply by droplets throughout shut interactions resembling coughing and speaking. It can even stay on some surfaces for days. During sure procedures, the virus becomes aerosolized and might linger in a room for longer intervals. In such circumstances, well being care staff are directed to take “airborne precautions” and put on N95 masks or one other type of respirator.
She stated she’s baffled by how unprepared the federal government and hospitals are for this second.
The day Jacklyn exhibits as much as the hospital and there are not any N95 masks, she stated, she’ll refuse to work.
“I’m not on a suicide mission here. I’m not going to do anything that puts my life at risk. What is my daughter going to do without me? What would my husband do without me?” she stated.
With a nationwide scarcity of protecting tools, many hospitals are limiting how typically nurses and medical doctors can get new masks and devising methods to stretch provides.
“Whoever is disinfecting these masks, are they trained to do this? Is someone supervising? Where are they doing it and how?” puzzled Sophia Rago, an ER nurse based mostly in St. Louis, about her hospital’s coverage.
Rago stated she will get just one surgical masks and one N95 masks for 3 shifts in a row. Afterward, she locations her gear in a brown paper bag and writes her identify on it.
“You give it to somebody and they are supposed to be disinfecting it between your shifts,” she stated. “Do I trust that? No! It can be disheartening to have that feeling of uncertainty that you are not going to be protected.”
Much of the anxiousness felt by front-line well being care staff stems from the ever-shifting federal steerage that in some circumstances later turned out to be unsuitable.
For instance, within the early days of the pandemic, the Centers for Disease Control and Prevention had narrow criteria for screening suspected coronavirus circumstances, which was later broadened because the virus unfold within the U.S.
The CDC still recommends, in circumstances the place N95s aren’t available, that a easy surgical masks will suffice for well being care staff until they’re doing procedures that trigger aerosol spray from the sufferers, resembling intubating somebody. It was solely final week that the company changed its guidelines and informed all Americans to cowl their faces with masks or material when in public.
Health care staff are distrustful of suggestions that, many stated, seem to err on the facet of lower than what they require for defense. They level to the CDC’s suggestion to make use of a bandana or scarf as a final resort if masks run out.
“I don’t care what the CDC guidelines say. If your nurses feel uncomfortable in a certain area, you should give them what they need,” stated Ramona Moll, a nurse who works at UC Davis Medical Center in Sacramento, California.
Moll stated she contracted COVID-19 in mid-March after treating a affected person suspected of getting contracted the coronavirus. She believes the publicity occurred when the older affected person with dementia turned combative and tried to chunk her. At the time, Moll was carrying a surgical masks, goggles, gloves and a robe, however no N95 masks. Her gear was consistent with CDC tips.
“The hospitals need to take responsibility for the fact that they did not take care of their nurses. They did not have N95s available,” she stated.
Her hospital disputes her account. Spokesperson Edwin Garcia stated there have been no COVID-19 sufferers on the hospital on the time and that it has “dedicated, full-time teams that are committed to infection prevention and keeping our employees safe.”
Grueling Shifts, Stress And Bruised Faces
The lack of protecting gear is one piece of a mosaic of stress that comes with caring for COVID-19 sufferers.
There are the 12- and 13-hour shifts in uncomfortable masks, the numerous unknowns of the illness and difficulties screening for it, the worry of getting contaminated or by accident infecting one other affected person and the disappointment of watching individuals die alone.
At an underresourced group hospital in Los Angeles, a nurse practitioner, Marie, has a plastic bag in her automotive during which she stashes her used N95s for the day her hospital could run out.
“I’ll spend the majority of my shift trying not to have a panic attack and then come home and fear going back to work,” she stated. “If this goes on for weeks and weeks and things only get worse, I just don’t know how I’m going to be able to handle it.”
She requested to make use of her center identify as a result of her hospital has warned workers to not converse publicly; some staff have been reprimanded for important social media posts.
Marie has misplaced three kilos in every week. Once she places her masks on throughout a shift, she gained’t take it off and, thus, avoids consuming. The bridge of her nostril is reduce open from carrying it on her face for hours at a time. The lack of preparation has her contemplating leaving nursing after the pandemic passes.
“I have dedicated my life to treating other people,” she stated. “And yet when I’m in need, I’m not provided with what I need. It’s like an abusive relationship.”
Health care staff throughout the nation and the globe are sharing selfies of their bruised faces from carrying N95 masks.
“It is a long six hours to be in all that gear,” stated Amanda Adams, a journey nurse who works at an ER within the New York City suburbs. “I try to put aside my emotions and cheer up the patients. Meanwhile, I am thinking, which one is going to give it to me and am I going to get sick?”
Once Infected, Who Takes Care Of The Health Care Worker?
Already, front-line staff are falling in poor health and feeling they’ve to decide on whether or not to threat their lives to save lots of others.
At least 40 U.S. well being care staff within the U.S. have died of COVID-19, in keeping with Medscape. Some of them had been younger and early of their careers.
“That also increases the fear. That it’s hitting young people,” stated Dr. Roy Akarakian, an ER resident at Henry Ford Hospital in Detroit. “I’m worried and afraid about the overall situation. This is something we’ve never seen before.”
Akarakian has already survived the virus — one in every of greater than 730 workers of the Henry Ford Health System who’ve examined postive since monitoring started on March 12.
In Seattle, Edward, an ICU nurse, stated he developed flu-like signs and shortness of breath final month, after treating COVID-19 sufferers. He determined to remain at dwelling out of warning, whereas he waited for his check outcomes. Seven days handed earlier than he realized he was optimistic.
“It was just really hard and nerve-wracking,” stated Edward who works at Swedish Medical Center, and is utilizing solely his first identify as a result of he’s afraid of dropping his job for talking publicly.
While in isolation and recovering, he was required to make use of his personal trip and sick time. After studying he had COVID-19, he stated, his employer “tried to pin those results on something outside the hospital” — most likely, Edward stated, as a result of the hospital supplies totally paid emergency administrative depart provided that you’ll be able to show you caught it on the job.
“I did not feel supported at all,” he stated. “Their main concern was trying to explain away my positive results as community-acquired.”
In a press release, Swedish stated “it’s grateful for our caregivers’ unwavering commitment to our patients and the selflessness they bring to work every day to ensure our patients and community are safe.”
Tiffany Moss, a hospital spokesperson, additionally famous Swedish supplies 80 hours of full-paid emergency time without work for staff affected by COVID-19 — regardless of the place they had been uncovered to the virus — however solely after contaminated workers exhaust trip and sick time.
When Edward acquired the inexperienced gentle to return to work, his co-workers appeared afraid to be close to him.
“When I would tell people, they would physically back away from me, they would question whether I should be at work,” he stated. “It was hard to go home at night and deal with those emotions.”
This story is a part of a partnership that features NPR and Kaiser Health News.
This story is a part of a partnership that features NPR and Kaiser Health News.
This story may be republished at no cost (details).
Will Stone: @WStonereports
Related Topics Health Industry Multimedia Public Health States Audio COVID-19 Doctors Emergency Medicine Hospitals New York Nurses src=”http://platform.twitter.com/widgets.js” charset=”utf-8″>