With medical provides in excessive demand, federal authorities say well being staff can put on surgical masks for defense whereas treating COVID-19 sufferers — however rising proof suggests the follow is placing staff in jeopardy.
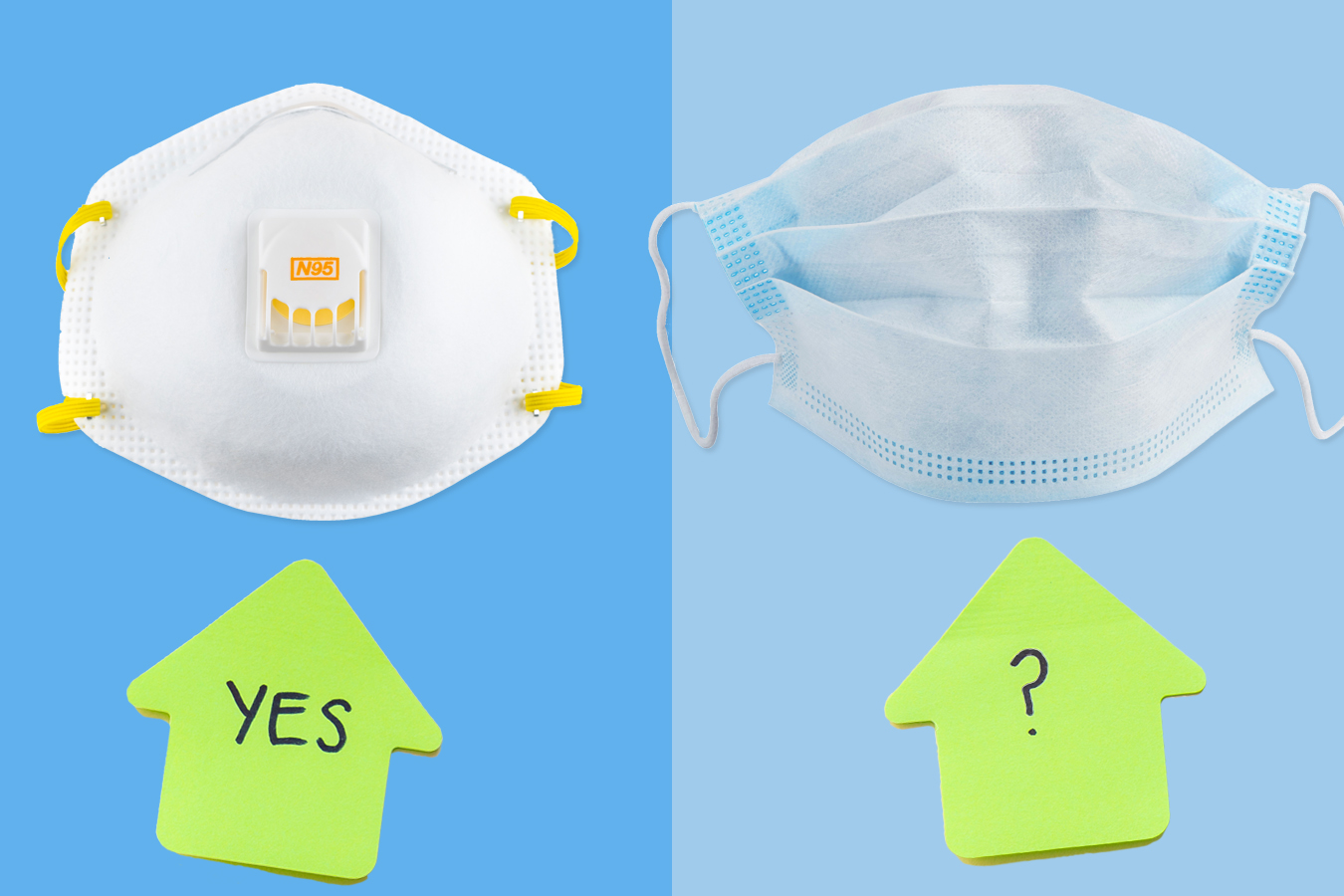
The Centers for Disease Control and Prevention lately mentioned lower-grade surgical masks are “an acceptable alternative” to N95 masks except staff are performing an intubation or one other process on a COVID affected person that might unleash a excessive quantity of virus particles.
But students, nonprofit leaders and former regulators within the specialised discipline of occupational security say counting on surgical masks — that are significantly much less protecting than N95 respirators — is sort of definitely fueling sickness amongst front-line well being staff, who possible make up about 11% of all recognized COVID-19 instances.
“There’s no doubt in my mind that that’s one of the reasons that so many health care workers are getting sick and many are dying,” mentioned Jonathan Rosen, a well being and security knowledgeable who advises unions, states and the federal authorities.
As of April 23, greater than 21,800 well being care staff had gotten the coronavirus and 71 had died, in accordance with a House Education and Labor Committee staffer briefed by the CDC.
The CDC’s recommendation contrasts with another CDC webpage that claims a surgical masks does “NOT provide the wearer with a reliable level of protection from inhaling smaller airborne particles and is not considered respiratory protection.”
Put merely, in employee security, “a surgical mask is not PPE,” or private protecting tools, mentioned Amber Mitchell, president and govt director of the International Safety Center and quick previous chair of the occupational well being and security part of the American Public Health Association.
The allowance for surgical masks made extra sense when scientists initially thought the virus was unfold by giant droplets. But a rising physique of analysis reveals it’s unfold by minuscule viral particles that may linger within the air as long as 16 hours.
A correctly fitted N95 will block 95% of tiny air particles — right down to three-tenths of a micron in diameter, which is the toughest to catch — from reaching the wearer’s face. But surgical masks, designed to guard sufferers from a surgeon’s respiratory droplets, aren’t efficient at blocking particles smaller than 100 microns, according to mask maker 3M Corp.
A COVID-19 particle is about 1 to four microns, in accordance with recent research.
Research from early April, inspecting two hospitals in South Korea, discovered surgical masks “seem to be ineffective in preventing the dissemination” of coronavirus particles. A 2013 Chinese research discovered that twice as many well being staff, 17%, bought a respiratory sickness in the event that they wore a surgical masks treating sick sufferers, in contrast with 7% of those that repeatedly used an N95, per the American Journal of Respiratory and Critical Care Medicine.
“My personal opinion would be, since there’s evidence of aerosol transmission, [at least] an N95 should be used for direct care of suspect or COVID-confirmed patients,” mentioned Dr. Robert Harrison, a doctor and professor on the University of California-San Francisco medical college who based UCSF Occupational Health Services.
In an emailed assertion, the CDC instructed that its steerage is supposed to preserve scarce assets and applies primarily to scarcity conditions.
Surgical masks must be used when N95s “are so limited that routinely practiced standards of care … are no longer possible,” mentioned Martha Sharan, an company spokesperson. “N95 respirators beyond their manufacture-designated shelf life, when available, are preferable to use of facemasks.”
Yet many well being amenities — citing the CDC pointers and scarce provide — are offering N95s in solely restricted medical settings.
Earlier this month, the nationwide Teamsters union reported that 64% of its well being care employee membership — which incorporates folks working in nursing houses, hospitals and different medical amenities — couldn’t get N95 masks.
At Michigan Medicine, the University of Michigan’s medical middle, staff don’t get N95s aside from performing particular procedures on COVID-positive sufferers — comparable to intubation or a bronchoscopy — or treating them within the intensive care unit, mentioned Katie Scott, a registered nurse on the hospital and vice chairman of the Michigan Nurses Association. Employees who in any other case deal with COVID-19 sufferers obtain surgical masks.
That matches CDC protocol however leaves nurses like Scott — who has learn the analysis on surgical masks versus N95s — feeling uncovered.
“We are at a risk of getting this virus, and we are at a risk of bringing it home to our families,” Scott mentioned. “It’s clear these surgical mask guidelines aren’t working.”
Nearly three,000 well being staff within the Detroit space — which incorporates Ann Arbor, the house of Michigan Medicine — have suspected or confirmed COVID-19 infections, in accordance with latest information reports.
At Michigan Medicine, staff can’t herald their very own protecting tools, in accordance with a criticism the nurses union filed with the Michigan Occupational Safety and Health Administration. Scott has PPE that her family and friends have mailed her, together with N95 masks. It sits at house whereas she cares for sufferers.
“To think I’m going to work and am leaving this mask at home on my kitchen table because the employer won’t let me wear it,” Scott mentioned. “You feel sacrificial in a way.”
News studies from Kentucky to Florida to California have documented nurses going through retaliation or strain to step down once they’ve introduced their very own N95 respirators.
A spokesperson for Michigan Medicine declined to reply questions in regards to the hospital’s protecting tools protocols. The American Hospital Association doesn’t have a stance on letting staff carry their very own N95s to work, mentioned Robyn Begley, the commerce group’s senior vice chairman and chief nursing officer.
In New York, the epicenter of the nation’s coronavirus outbreak, nurses throughout the state report receiving surgical masks, not N95s, to put on when treating COVID-19 sufferers, in accordance with a court docket affidavit submitted by Lisa Baum, the lead occupational well being and security consultant for the New York State Nurses Association.
“A surgical mask is not a form of PPE. … [If you] cough or sneeze, it catches some of the virus. It does not protect the wearer,” Baum mentioned in an interview with Kaiser Health News.
So far, at the very least 16 NYSNA members have died from the coronavirus, at the very least 94 have been hospitalized and greater than 1,000 have examined optimistic, in accordance with union estimates.
National Nurses United has pushed Washington lawmakers to cross laws that might ramp up manufacturing of N95s by compelling the White House to invoke the Defense Production Act, a Korean War-era regulation that enables the federal authorities, in an emergency, to direct private business in the production and distribution of goods.
It can also be calling on Congress to require that the Occupational Safety and Health Administration put forth an emergency short-term normal to mandate that employers present well being care staff with protecting tools, together with N95 masks, once they work together with sufferers suspected to have COVID-19.
“The employer has a responsibility to protect their employees,” mentioned Amirah Sequeira, the union’s lead legislative advocate. “At the same time, when you have a crisis at this scale, the federal government also has a responsibility to ensure the very increase in purchasing, and, if not purchasing, production.”
The AHA has lobbied towards a mandate that might increase use of N95s. Begley acknowledged that “supplies are inadequate” and mentioned heightened international demand makes getting N95s way more troublesome.
“If we fail to conserve already limited supplies, there will be no N95s remaining for health care staff performing aerosolizing procedures,” Begley mentioned.
But the failure to get extra and higher protecting gear to well being staff might value extra lives, union leaders warned in a latest teleconference in regards to the harmful circumstances staff are going through.
“Nurses are not afraid to care for our patients if we have the right protections,” mentioned Bonnie Castillo, the chief director of National Nurses United, “but we’re not martyrs sacrificing our lives because our government and our employers didn’t do their job.”