Masks, gloves and different gear are essential as well being care staff face the COVID-19 outbreak. There is a strategic nationwide stockpile that the U.S. authorities controls — however nobody is aware of what, past that stockpile, is accessible within the non-public sector.
Some hospitals have a surplus of the protecting gear and a few not sufficient. The Centers for Disease Control and Prevention is engaged on a system that will observe the stock throughout the U.S.
The large hurdle isn’t the know-how. The subject is getting hospitals comfy sharing details about their preparedness — data that, till now, they’ve thought of confidential.
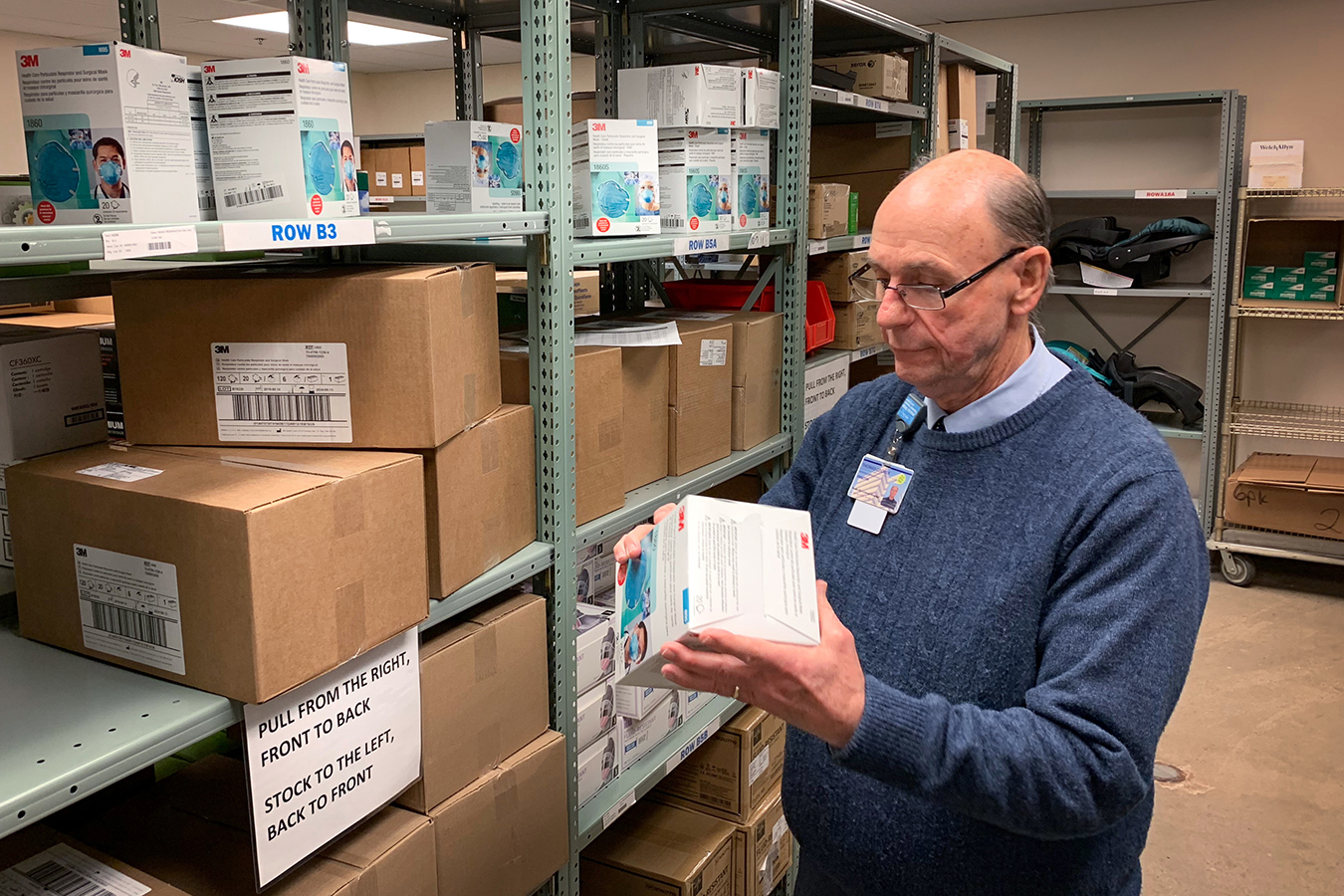
Protective masks have develop into a scorching commodity, even inside hospitals. At Nashville General Hospital, for instance, workers a number of weeks in the past have been casually approaching provide chain administration director Tom Cooper and asking if they may have a field for private use.
Cooper advised them the masks have been obtainable just for “clinicians as needed, for their job duties.”
And Cooper mentioned he’s feeling extra protecting of the provision his hospital has available — particularly N95 respirators. General Hospital’s distributor, Medline, already restricted orders of the respirators. Cooper mentioned he can’t get any greater than his common month-to-month allotment, even when he might afford it.
“Right now, we’re OK,” he mentioned. “But next month, what could happen?”
Email Sign-Up
Subscribe to KHN’s free Morning Briefing.
‘Panic Purchasing’
The CDC has tried to keep away from such shortage and the prices related to shortages. Often, there’s loads of disposable protecting gear to go round, but it surely’s not all the time in the precise locations forward of pandemics.
“It can result in ‘panic purchasing,’” mentioned Megan Casey, a nurse epidemiologist with the CDC. “This is where facilities buy as much as possible, just to be on the safe side.”
Right now, public well being companies know solely what’s in authorities stockpiles of protecting gear. Health and Human Services Secretary Alex Azar advised Congress in current weeks that the federal government has 30 million masks, though 300 million could also be wanted. (The few U.S. corporations manufacturing masks say demand in current weeks has far outstripped their production capability, although they’re ramping up.)
The nation’s 6,000 hospitals have been extra of a black field — now and in earlier epidemics. In previous outbreaks — of H1N1 influenza, for instance — some hospitals resorted to casual provide swaps on a avenue nook, based on challenge managers with the Center for Medical Interoperability, a Nashville-based nonprofit.
Last yr, earlier than COVID-19 emerged, the middle was awarded a $three million contract with the CDC to construct a system that requires hospitals to submit details about their real-time stock. The data sometimes could be pulled instantly from an establishment’s digital medical document system. Using that gathered knowledge, the CDC ought to be capable to use a digital dashboard to simply determine services with the best want.
“It could also, potentially, provide a tool for hospitals to request personal protective equipment from state or local health departments, stockpiles or even other hospitals that might have excess,” Casey mentioned. “We do see this as a potential opportunity for resource sharing and having those kinds of discussions.”
A storage closet within the basement of Nashville General Hospital holds hardly ever used protecting fits. Melanie Thomas, chief data officer on the hospital, is now sharing data with the CDC about its stock of this form of gear.(Blake Farmer/WPLN)
Competitive Advantage
But the prospect of sharing provides is the place the enterprise of well being care makes cooperation arduous even in a disaster, mentioned Melanie Thomas. She’s the chief data officer at Nashville General, one of many pilot websites for the CDC-sponsored challenge.
“It’s difficult and scary sometimes to share data and equipment, especially with your competitors,” Thomas mentioned, “because you want to have the advantage.”
Nashville General is the smallest of the pilot websites, which embody Northwestern Memorial in Chicago and Nashville-based Community Health Systems, a for-profit chain of almost 100 hospitals across the U.S.
Thomas acknowledged it’s simpler for her taxpayer-funded hospital to grant entry to its stock system as a result of it doesn’t have the shopping for energy to stockpile gear.
“That’s never going to be our problem,” she mentioned. “We want the shared information because we’re going to have just enough.”
And after they run out, she’d wish to know the place to show to get extra.
A Theoretical Threat Becomes Real
The Center for Medical Interoperability began its work quietly, just a few months earlier than COVID-19 emerged. But the challenge managers have observed a larger willingness to take part amongst main well being programs now that a theoretical menace has develop into very actual.
“We know … that their supply chains are under strain right now because these products, they come out of China,” mentioned Tommy Ragsdale, the middle’s director of technique.
China wants the disposable gear that’s manufactured there for its personal use. And solely a handful of corporations within the U.S. nonetheless make the protecting gear domestically. One has orders for greater than a billion masks.
“It has definitely created different discussions at the hospital and health system level than we were having in October or November,” Ragsdale mentioned.
The CDC has pumped an extra $600,000 into the data-sharing challenge, with an accelerated go-live date in May, Ragsdale mentioned. The heart plans to carry a webinar on April 1 for added hospitals fascinated with taking part in later phases.
At this level, the CDC mentioned, there’s no mandate for hospitals to take part. But Ragsdale mentioned he hopes they are going to see the profit: “This is clearly for the greater good.”
This story is a part of a partnership that features Nashville Public Radio, NPR and Kaiser Health News.
Blake Farmer, Nashville Public Radio: [email protected]”>[email protected], @flakebarmer
Related Topics Public Health States CDC COVID-19 Hospitals src=”http://platform.twitter.com/widgets.js” charset=”utf-Eight”>