This story additionally ran on Vice. This story might be republished without cost (details).
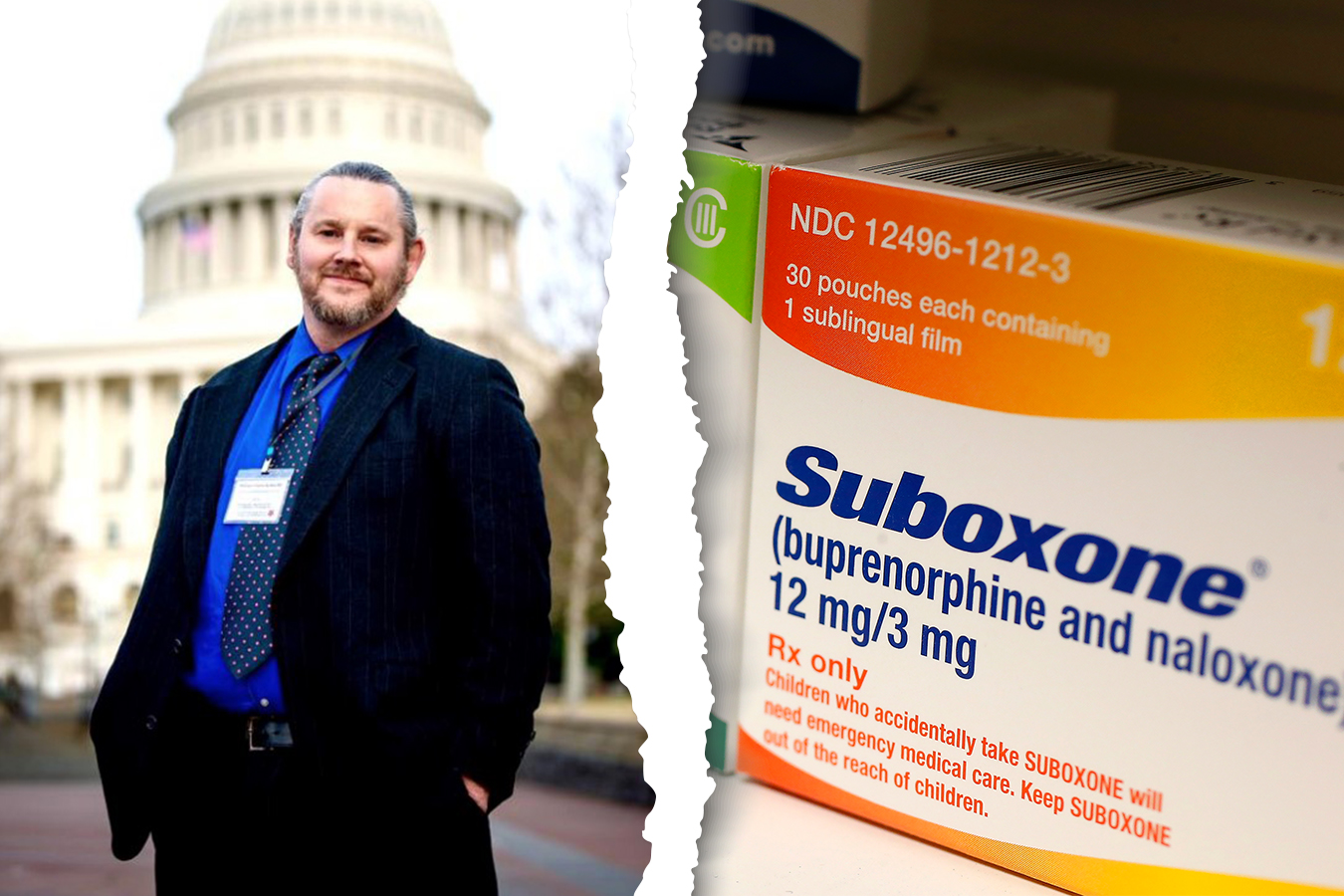
Dr. Wesley Boyd, an affiliate professor of psychiatry at Harvard, has spent years working with state applications that assist docs, nurses and different well being care staff who’ve develop into hooked on opioids get again on their toes professionally.
He helps these non-disciplinary applications, wherein docs and nurses enroll for quite a few years and are carefully monitored by habit specialists and state authorities as they search to keep up or restore their medical licenses. But, he mentioned, he’s perplexed as to why these applications and different efforts to assist well being care suppliers usually don’t stress a restoration methodology that has lengthy been proven to be efficient: the usage of medicine like buprenorphine and methadone, referred to as opioid agonists, to alleviate cravings.
“Obviously the data are clear that medication-assisted treatment is the best course of action,” mentioned Boyd, who labored for Massachusetts’ Physician Health Services (beforehand referred to as the Society to Help Physicians) from 2004 to 2010. “Whether they’re doctors, nurses or anybody else, [they] can function perfectly well at work and in their lives generally while they’re using medication-assisted treatment.”
Furthermore, he mentioned, “the odds that they’re going to stay clean and sober while using medications for treatment are better.”
Clinical studies present medication-assisted treatment considerably decreases the rate of relapse and overdose greater than different interventions alone. Most advocates advise utilizing it along with common remedy or counseling. Legal and medical researchers additionally made this level within the New England Journal of Medicine final month, calling it “ironic that clinicians, who are better positioned than most people to acquire and afford opioid-agonist therapy, are often denied it.”
Email Sign-Up
Subscribe to KHN’s free Morning Briefing.
But some well being care professionals imagine opioid agonists are simply an alternative to the medicine a health care provider is hooked on, and, since they bind to the identical mind receptors as opioids, could have an effect on suppliers’ skill to do their jobs. The opioid agonists assist cut back relapses and cravings by stimulating the identical pathways opioids do, however in a managed method that stops an individual from feeling excessive.
Non-Disciplinary Treatment Programs For Addiction
Non-disciplinary therapy applications have been working in most states because the 1970s to assist well being professionals overcome their habit. Instead of revoking the license of a person who’s discovered to be impaired on the job, these peer-run applications attempt to get individuals again to work with mandated therapy plans that embody intensive remedy, monitoring their habits out and in of the office and, after all, drug testing. Throughout therapy, individuals are actively discouraged, if not outright banned from, utilizing opioid agonists that would assist their restoration.
Members of the non-disciplinary program could advocate for a participant’s return to work after they imagine the person is prepared, however, in the end, it’s the state board that determines when a person is match to look after sufferers.
Bill Kinkle, a registered nurse in Pennsylvania, developed an habit to opioids greater than a decade in the past and misplaced his license. He tried a number of restoration applications however relapsed and overdosed a number of occasions.
He has been working with the state’s Peer Nurse Assistance Program to get his license again. When he requested if he may use Suboxone, a model title for a mix of buprenorphine and naloxone, he was instructed that the nurse help program wouldn’t permit it except he had an in depth plan for truly fizzling out the drug.
So he’s treating his habit by way of the state program with out the medicine. He was required to take part in a 30-day inpatient program, endure partial hospitalization (wherein a participant is handled for a number of hours a day however can go house within the evenings) for an extra three weeks, obtain three months of intensive outpatient remedy, attend Alcoholics Anonymous conferences three to 5 occasions per week and pay for costly random urine screenings.
The Peer Nurse Assistance Program didn’t reply to requests for remark.
Some state officers are starting to contemplate the usage of medicine like methadone and buprenorphine. The North Carolina Medical Board, which handles doctor licensing and self-discipline, is encouraging the state program for docs with opioid addictions to introduce these drugs.
Critics argue that the non-disciplinary applications can, in reality, really feel extra disciplinary than supportive and don’t assist as many individuals as they might if opioid agonists have been made obtainable.
The applications “have no independent oversight and patients don’t have a recourse,” mentioned Dr. Peter Grinspoon, an internist in Boston who had an opioid habit and was each a participant in, and finally a board member of, Massachusetts’ Physician Health Services program for addicted docs.
Grinspoon, who additionally teaches at Harvard, mentioned that though he was unaware of any formal state coverage towards medication-assisted therapies, not one of the program’s individuals with opioid addictions used opioid agonists whereas he served.
Impairment in Safety-Sensitive Positions
Scott Teitelbaum, medical director on the University of Florida Recovery Center, which treats well being care professionals from everywhere in the nation, mentioned he generally prescribes the medicines to the half of his sufferers who don’t work in “safety-sensitive positions.”
But, he mentioned, it is smart to have a distinct technique for sufferers in these positions. When the applications ask him if an individual ought to return to observe, they’re not asking what’s finest for the person; they’re asking whether or not it’s secure for the general public. And when sufferers are utilizing agonist therapies, Teitelbaum, who additionally was handled for cocaine and marijuana use, mentioned he isn’t positive it’s.
A review in Mayo Clinic Proceedings of a number of research in 2012 confirmed small results of each methadone and suboxone on efficiency in measures similar to response time and reminiscence. The review was criticized for weak evidence and an absence of applicable management teams.
Grinspoon famous that docs might be taking different drugs that have an effect on their efficiency however face no repercussions. For instance, he mentioned, they might take benzodiazepines for nervousness or Ambien to assist them sleep.
“There are tons of pharmaceuticals that could affect our performance — all of which doctors are allowed to take,” he mentioned. “And it’s just because of the stigma that they’re singling out addiction.”
Success Rates
Critics of medication-assisted therapy typically level to the overwhelming five-year success charges reported by the non-disciplinary applications — usually between 70% and 90%.
But Boyd is cautious of these rosy statistics. First, he famous, they hardly ever rely individuals who dropped out of this system or died by suicide. He mentioned some professionals who by no means suffered from substance use dysfunction are compelled into this system by unhealthy evaluations.
So far, Kinkle, the nurse in Pennsylvania, has stayed on monitor, “white-knuckling it” with out Suboxone. If all goes based on plan, his license will likely be reinstated in one other 13 months.
“My wife found me multiple times after an overdose lying on the floor unconscious,” mentioned Kinkle. “All that could have been prevented had I been offered” Suboxone.
This story additionally ran on Vice. This story might be republished without cost (details). Related Topics Health Industry Public Health States Doctors Nurses Opioids Substance Abuse